Higher Amputation And Lower Reintervention Rates Observed In Frail Peripheral Artery Revascularization Patients Regardless Of Initial Approach
Elizabeth L. George, MD1, Aditi Kashikar, MD1, Kara A. Rothenberg, MD2, Nicolas B. Barreto, MS1, Manjula K. Tamura, MD1, Amber W. Trickey, PhD, MS3, Philip P. Goodney, MD4, Shipra Arya, MD, SM1.
1Stanford University, Stanford, CA, USA, 2UCSF East Bay, Oakland, CA, USA, 3Stanford University, Palo Alto, CA, USA, 4Darthmouth-Hitchcock Medical Center, Lebanon, NH, USA.
Introduction: Given the expanding armamentarium of catheter-based options for peripheral arterial disease (PAD), our high-risk patients merit special consideration in the “endo vs open” debate; however, the relationship between frailty and limb preservation remains unknown. Thus, we evaluated the association of frailty with major adverse limb events (MALE) after infra-inguinal bypass (open-bypass) and endovascular peripheral vascular interventions (endovascular-PVI).
Methods: The 2011-2017 Vascular Quality Initiative (VQI) database was queried to categorize patients undergoing open-bypass or endovascular-PVI without prior interventions. Frailty was measured using the VQI-Risk Analysis Index (VQI-RAI): gender, BMI, kidney disease, congestive heart failure, dyspnea, living status, and activities of daily living. Frailty was dichotomized into “frail” (RAI≥35) and “non-frail” (RAI<35) per prior work. The primary endpoint was MALE: a composite outcome of ipsilateral amputation and need for target lesion revascularization (TLR). Associations of frailty and procedure type with MALE, amputation, and TLR up to15 months were estimated using logistic regression models adjusted for race, insurance type, smoking, diabetes, and presentation (claudication, rest pain, or tissue loss).
Results: In total, 38,987 patients underwent procedures for PAD; 25,053 (64.3%) had sufficient follow-up data [mean age: 68.3 years (SD 11.3); 38.5% female]. Of these, 8,173 (32.6%) patients underwent open-bypass initially [mean RAI 36.8 (SD 7.0)], while 16,880 (67.4%) underwent endovascular-PVI [mean RAI 37.7 (SD 7.1), p<0.001]. Overall, 63.3% of patients were classified as frail. MALE occurred in 5,368 (21.4%) unique patients [TLR 4,585 (18.3%) and amputation 1,336 (5.3%)]. In adjusted logistic regression, frailty was not associated with MALE (OR 0.94; 95% CI [0.86-1.02], p=0.12), but was significantly associated with higher odds of amputation (1.45; [1.24-1.71], p<0.001) and lower odds of TLR (0.89; [0.82-0.97], p=0.01) [Figure 1]. Even when adjusting for frailty, patients first undergoing open-bypass were significantly more likely to experience MALE (OR 1.39; 95% CI [1.25-1.53], p<0.001), amputation (1.60; [1.30-1.95], p<0.001), and TLR (1.46; [1.31-1.62], p<0.001).
Conclusion: Frailty is associated with a higher odds of amputation and lower odds of reintervention after PAD procedures. An “open first” approach was significantly associated with higher adverse limb events. Further research is needed regarding choice of initial and repeat interventions in frail/high-risk patients. 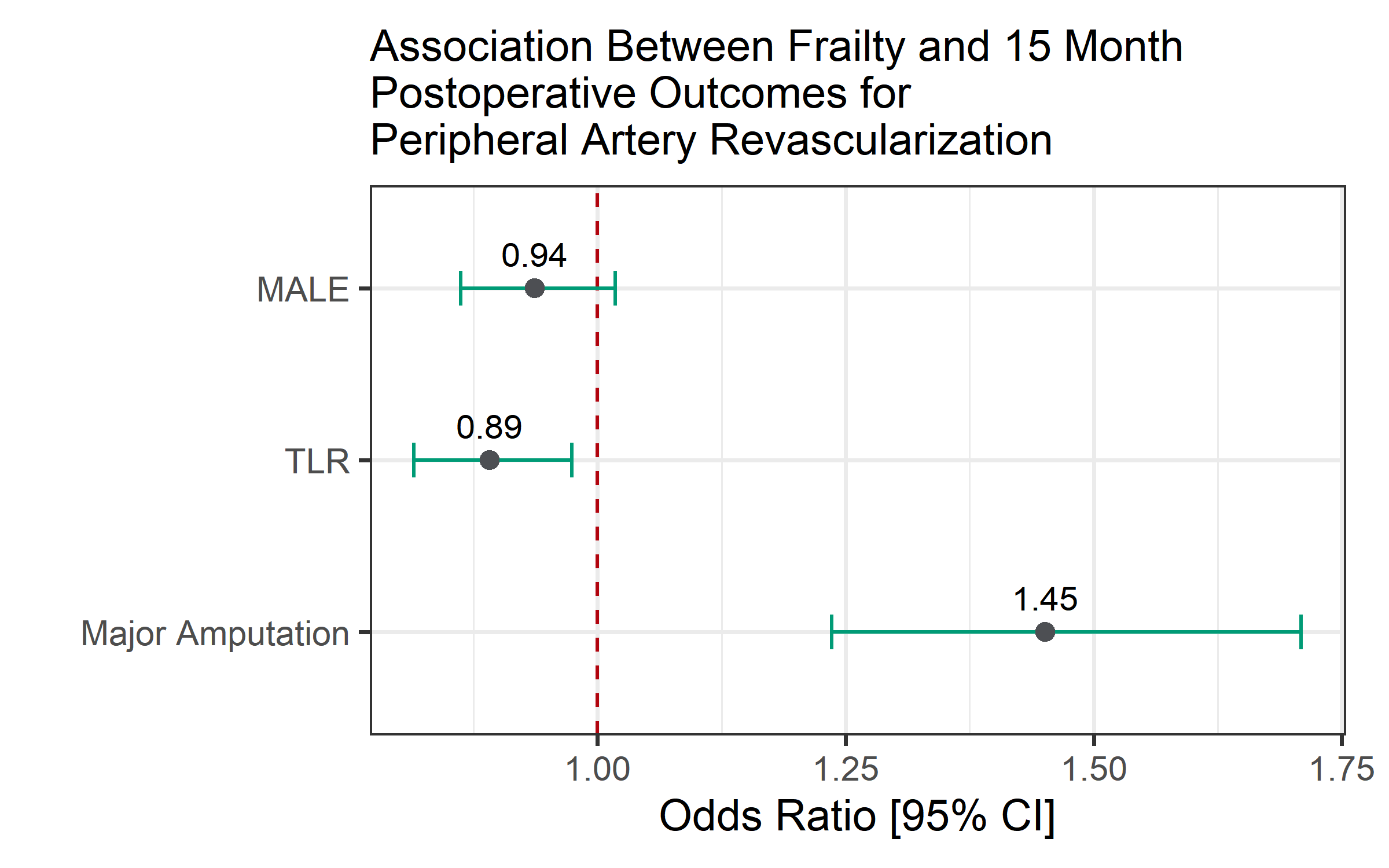
Back to 2020 ePosters
