Outcomes Of Lower Extremity Revascularization Among Patients With Human Immunodeficiency Virus
Tanner Kim, MD1, Anand Brahmandam, MBBS1, Timur Sarac, MD2, Kristine Orion2.
1Yale University School of Medicine, New Haven, CT, USA, 2Ohio State University College of Medicine, Columbus, OH, USA.
OBJECTIVES: The development of highly active antiretroviral therapy (HAART) has significantly improved the life expectancy of patients with human immunodeficiency virus (HIV). However, this increased longevity has given rise to a number of chronic conditions including peripheral arterial disease (PAD). The aim of this study was to investigate the trends and outcomes of lower extremity revascularization (LER) among HIV positive patients with PAD.
METHODS: The National Inpatient Sample (NIS) was reviewed between 2004 –2014. All hospital admissions with a diagnosis of PAD undergoing LER were stratified based on HIV status. Demographic data, comorbidities, rates of interventions, rates of inpatient mortality and limb loss were analyzed. Propensity score weighting was then performed based on demographics and comorbidities to compare outcomes. Linear regression was used to analyze trends over time.
RESULTS: During the study period, there were 9,513 (0.29%) HIV positive patients with PAD who underwent LER (Table 1). Patients with HIV were more likely to be younger, male and African American. They were also more likely to have fewer comorbidities including coronary artery disease and present with chronic limb threatening ischemia. HIV positive patients were more likely to undergo open LER as compared with those without HIV (HIV= 40.60% vs no-HIV = 35.28%; p<0.01). There was a significant increase in the proportion of patients with HIV undergoing intervention for PAD over this time period from 0.25% to 0.42% (p<0.01). HIV positive patients had significantly greater length of stay and total hospital costs (p<0.01). There was no difference in rates of inpatient limb loss (HIV=11.40% vs no HIV = 10.42%, p=0.13). Inpatient mortality was significantly lower among HIV positive patients (HIV = 1.93% vs no HIV 3.54%, p<0.01). After propensity score weighting, there was no significant difference in inpatient limb loss (OR: 1.04, CI: 0.27-4.08) or inpatient mortality (OR: 0.91, CI: 0.18-4.53).
CONCLUSIONS: LER is safe for HIV positive patients without increased risk of periprocedural limb loss or mortality. HIV positive patients are younger and have fewer comorbidities, but have increased length of stay and costs. The proportion of HIV positive patients undergoing LER in a hospital setting continues to increase. 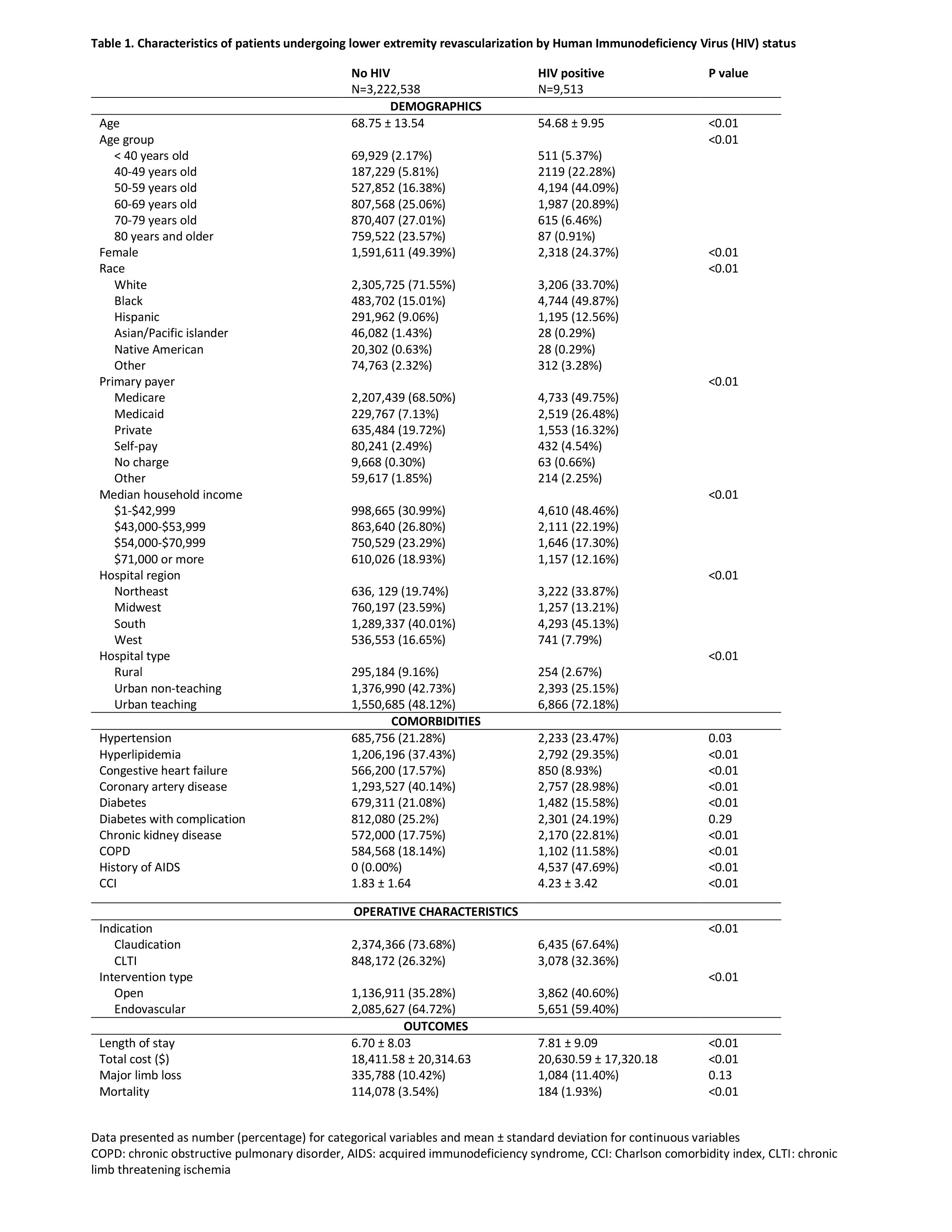
Back to 2020 ePosters
