Comparative Outcomes Of Antegrade And Retrograde Debranching For Hybrid Repair Of Thoracoabdominal Aortic Aneurysms
Dean J. Arnaoutakis, MD, MBA, Craig T. Elder, MD, Salvatore T. Scali, MD, Kristina A. Giles, MD, Eric Y. Pruitt, MD, Amanda C. Filiberto, MD, Michol Cooper, MD, PhD, Scott A. Berceli, MD, PhD, Thomas S. Huber, MD, PhD, Martin Back, MD, Gilbert R. Upchurch, Jr., MD.
University of Florida, Gainesville, FL, USA.
Objective: Open repair of thoracoabdominal aortic aneurysms(TAAA) is associated with significant morbidity and mortality. Hybrid repair has emerged as an alternative, less-invasive strategy whereby proximal thoracic endovascular aortic repair(TEVAR) is combined with either an antegrade open paravisceral aortic repair or retrograde open aorto-iliac visceral/renal debranching. Outcomes comparing these hybrid techniques are poorly described. The purpose of this analysis was to compare outcomes of these two hybrid strategies in the management of TAAA while controlling for variables that influence risk of postoperative outcomes.
Methods: All TAAA patients with non-mycotic, degenerative aneurysm, pseudoaneurysm, or chronic dissection with aneurysm undergoing hybrid TAAA repair(2003-2019) at a single institution were examined. Primary endpoint was 30-day mortality. Secondary endpoints included incidence of in-hospital major complications and 90-day re-admission. Inter-group comparisons were made using crude and risk-adjusted analyses. Kaplan-Meier analysis estimated freedom from re-intervention and overall survival.
Results: Sixty-one patients(mean age-68±12 years; 66%-male; aneurysm diameter-66±11mm) were identified with 17(28%) undergoing an antegrade approach and 44(72%) undergoing retrograde debranching. Comorbidities were prevalent(coronary disease-51%, hypertension-92%, COPD-50%, smoking-85%) with no differences between groups. Patients undergoing antegrade approach were more likely to have prior aortic dissection with aneurysm formation(35% vs. 2%;p=.001) and more extensive aneurysm disease(extent II/III-83% vs. 68%;p=.015) compared to retrograde debranching. No difference in staged repairs was present(antegrade-94% vs. retrograde-77%;p=.15).
Overall 30-day mortality was 15% with the antegrade cohort having a significantly decreased rate(0%) compared to the retrograde approach(20%;p=.04). Any complication developed in 47% with no difference between groups. Permanent spinal cord ischemia(SCI) was significantly more prevalent in the antegrade subset[25%(n=4) vs. 6%(n=2);p=.04]. After risk-adjustment, age(HR 2.36;p=.002) and aneurysm diameter(HR 1.76;p=.001) increased risk of death, whereas preoperative aspirin use was protective(HR .33;p=.005). Freedom from aortic re-intervention was similar between the two strategies(log-rank p=.595) as was overall survival(log-rank p=.69)(Figure).
Conclusions: Complications following hybrid TAAA are common and are not differentially associated with a specific hybrid strategy. Despite being used more frequently for more complex TAAA disease and having a higher rate of permanent SCI, an antegrade approach was associated with better 30-day mortality compared to retrograde debranching. However, this short-term improvement did not translate into long-term re-intervention or survival benefit. 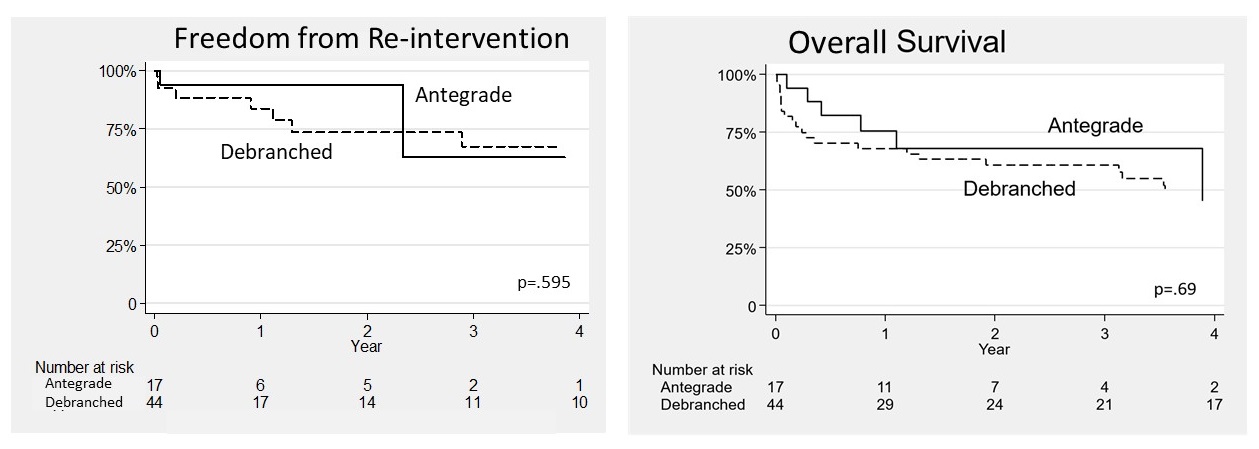
Back to 2020 ePosters
