A Novel Method Of Quantifying Perfusion In Peripheral Arterial Disease Using Thermal Imaging
Jonathan Bath, Hasanain O. Al-Sadr, MSc, Mihai Popescu, PhD, Todd R. Vogel, MD.
University of Missouri, Columbia, MO, USA.
Objective: Peripheral arterial disease (PAD) is evaluated with clinical examination and ankle-brachial indices (ABI). Methods to estimate perfusion can be inaccurate in situations of non-compressible arteries or in patients with wounds and can be invasive. We describe the clinical application of thermal imaging in PAD before and after intervention.
Methods: Patients with PAD who were scheduled for endovascular or open procedures were enrolled prospectively. Thermal imaging was undertaken immediately pre- and post-intervention and at 1 month follow-up using a FLIR A320 IR camera. Patients were imaged from the knee to the foot to create temperature profiles with Gaussian Process Regression used to model the min, max, mean and median temperatures against the ABI.
Results: Twelve patients with PAD were enrolled in the study, mostly male (70%). Mean age was 64 (± 7.4) and six right and six left legs were treated. Endovascular procedures were performed in ten patients (83%) with one left axillary to femoral bypass and one right femoral endarterectomy with iliac and SFA stenting in another. Indications for surgery were: claudication in 4 patients (33%), rest pain in 6 patients (50%) and tissue loss in 2 patients (17%). For all cases there was a high level of correlation between the pre-, post-intervention and 1-month follow-up thermal imaging and ABI, with mean R-Squared value of 0.83. Immediately following successful intervention (Figure 1.) there was a significant increase in mean target limb temperature when compared with pre-intervention (32.9 degrees Celsius vs. 32.2 degrees Celsius; p < 0.005).
Conclusions: Thermal imaging provides an immediate, simple and reliable quantification of perfusion that correlates highly with the ABI. Prior to this study the accuracy of thermal imaging for perfusion in PAD was unknown, which limited the clinical applicability of this technology. Additional clinical uses may include real-time monitoring of bypass or stent patency, free flap viability or wound healing in the patient’s home environment using a smartphone-enabled thermal camera. This may offer significant advantages in healthcare cost-savings and adherence to follow-up over hospital-based monitoring. Further study of thermal imaging in assessing perfusion in these diverse clinical settings is planned. 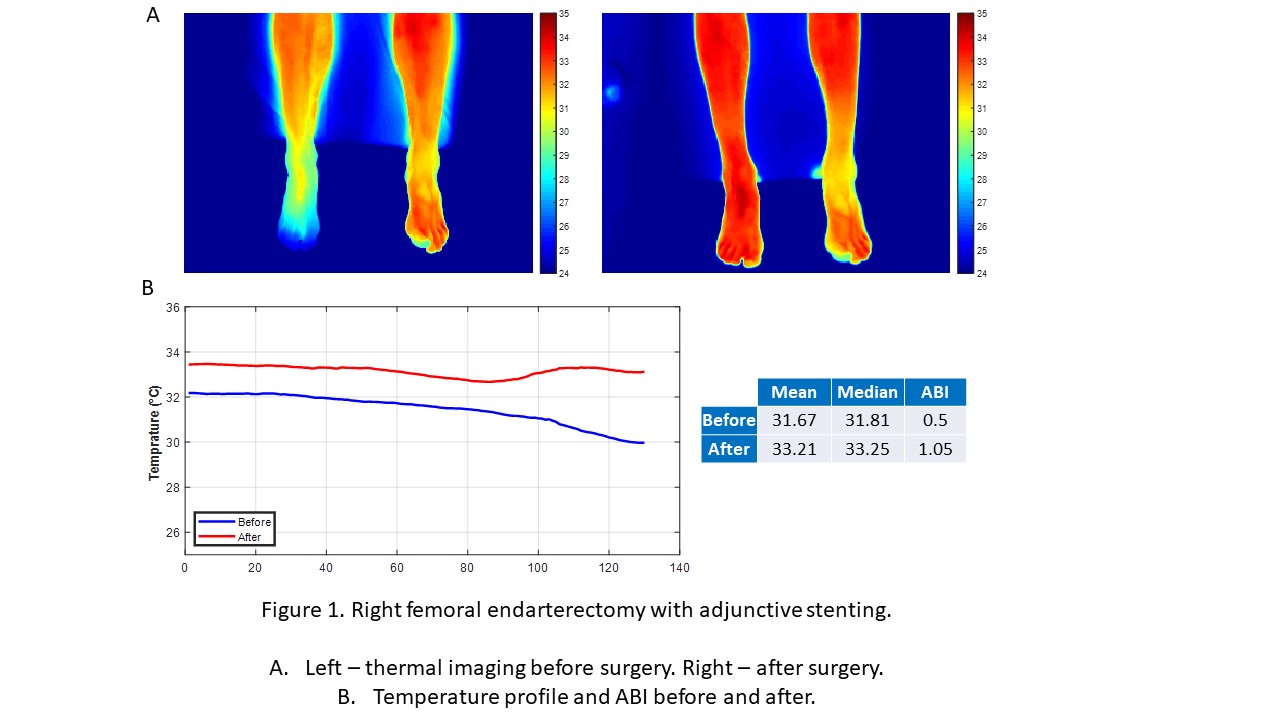
Back to 2020 ePosters
