The Impact Of Clamp Location On Outcomes Following Open Juxtarenal Aneurysm Repairs
Ambar Mehta, MD, MPH1, Thomas F. O’Donnell, MD2, Richard Schutzer, MD1, Eric B. Trestman, MD1, Karan Garg, MD3, Jahan Mohebali, MD, MPH2, Jeffrey Siracuse, MD4, Marc Schermerhorn, MD5, William D. Clouse, MD6, Virendra Patel, MD, MPH1.
1Columbia University Medical Center, New York, NY, USA, 2Massachusetts General Hospital, Boston, MA, USA, 3NYU Lagone Medical Center, New York, NY, USA, 4Boston University Medical Center, Boston, MA, USA, 5Beth Israel Deaconess Medical Center, Boston, MA, USA, 6University of Virginia, Charlottesville, VA, USA.
OBJECTIVES: Despite the increasing prevalence of juxtarenal abdominal aortic aneurysms (AAAs), surgical approaches for open repairs continue to vary, especially regarding placement of the proximal aortic clamp. This study assessed whether placing a proximal clamp above both renal arteries versus a single one was associated with worse postoperative renal dysfunction and 30-day mortality.
METHODS: We used the 2004-2018 Vascular Quality Initiative to identify all patients undergoing open repairs of non-ruptured juxtarenal AAAs and compared outcomes by clamp site: above one renal artery, above both renal arteries (supra-renal), or above the celiac trunk (supra-celiac). Outcomes included acute kidney injury (AKI, defined as creatinine increase >0.50 mg/dL), new-onset renal failure requiring renal replacement therapy (RRT), and 30-day mortality. We used multilevel logistic regressions, clustered at the hospital level, to adjust for confounding.
RESULTS: We identified 3734 patients (median age 71 years, 70% male, 92% Caucasian), where the median aneurysm diameter was 5.9cm (IQR 5.4-6.8cm). Proximal clamp sites varied: above one renal artery (31%), supra-renal (52%), and supra-celiac (17%). Overall, 30-day mortality was 4.8%, AKI was 20%, and new-onset RRT was 4.0%. Compared to clamping above a single renal artery (Table), supra-renal clamping was associated with increased odds of AKI (OR 1.41 [1.18-1.68]) but not new-onset RRT (OR 1.27 [0.75-2.14]) or 30-day mortality (OR 1.01 [0.69-1.48]). In contrast, supra-celiac clamping was associated with higher odds of both AKI (OR 1.36 [1.01-1.85]) and new-onset RRT (OR 2.00 [1.28-3.12]) and trended towards greater 30-day mortality (OR 1.51 [0.99-2.30]). Every 10-minute increase in intraoperative renal ischemia time raised the odds of all three outcomes: AKI by 7% (3%-11%), new-onset RRT by 11% (5%-17%), and 30-day mortality by 10% (4%-16%).
CONCLUSIONS: For patients undergoing open repairs of juxtarenal AAAs, supra-renal clamping relative to clamping above a single renal artery was associated with AKI but not new-onset RRT or 30-day mortality. However, intraoperative renal ischemia time was independently associated with all three postoperative outcomes. Certain patients may benefit from supra-renal clamping versus clamping above a single renal artery if it decreases intraoperative renal ischemia time, for lower rates of new-onset RRT and 30-day mortality. 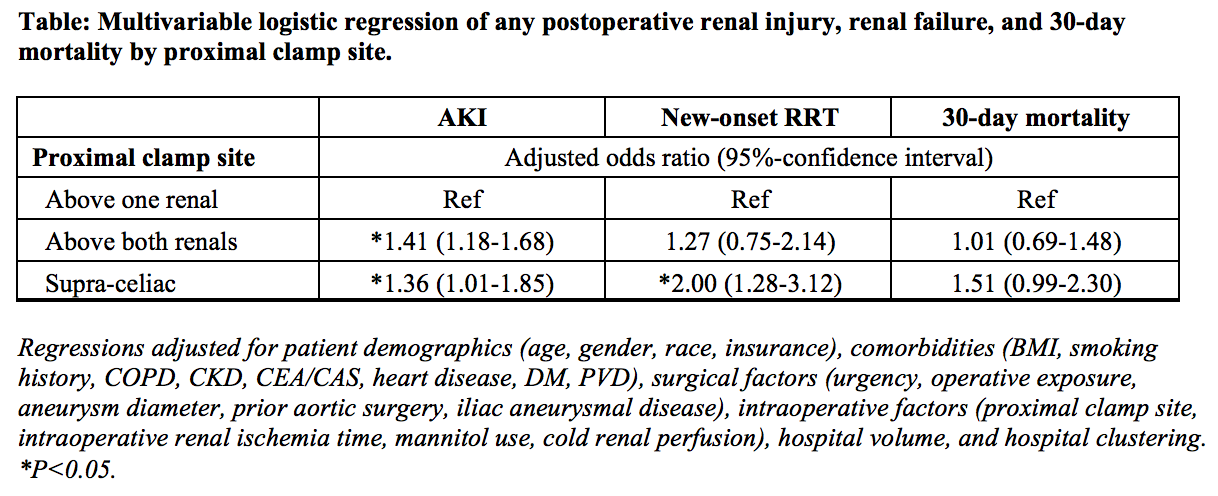
Back to 2020 ePosters
