'Have Stroke, Will Travel': Patient Access To High-Volume Surgeons For Carotid Endarterectomy
Ina Y. Soh, MD1, Stephen J. Tarsa, PhD2, Matthew D. Breite, MD1, William W. Sheaffer, MD1, Victor J. Davila, MD1, William M. Stone, MD1, Samuel R. Money, MD1, Andrew J. Meltzer, MD1.
1Mayo Clinic, Phoenix, AZ, USA, 2Harvard University, Cambridge, MA, USA.
OBJECTIVES: Multiple studies demonstrate superior outcomes when high-risk surgery is performed by high-volume surgeons. This impacts referral patterns, hospital credentialing and public policy. The Leapfrog Group, for example, recommends a “minimum volume standard” for procedures such as carotid endarterectomy (CEA). One potential downside of such mandates is the impact on patient access to surgical care. The purpose of this study is to characterize patient access to surgeons meeting the Leapfrog Group standards for CEA (ten cases per year), and to model the impact of disease prevalence and workforce changes on access to these high-volume surgeons (HVS).
METHODS: 2012-2017 medicare provider utilization data was used to identify HVS performing >=10 CEA annually. Surgeon location was resolved to latitude-longitude coordinates using the Google Maps GeoCoding service. Average driving times were estimated using counties' geographic centers of population per U.S. Census Bureau. Driving times reflect the fastest route accounting for road network and speed limit, based on data from the Open Street Maps project and the Open Source Routing Machine's hierarchy-contraction algorithm. Driving times to second and third-closest HVS modeled future access to care as surgeon attrition continues.
RESULTS: Regression analysis demonstrated 3,076 fewer CEA per year and 103 fewer HVS per year. Despite this, 92.5% of the U.S. population resides within a 1-hour drive to an HVS (Figure 1). HVS consolidation between 2012-2017 led to loss-of-access for 1.4% of the U.S. The largest loss occurred in New York, Wisconsin, Missouri, Arkansas, and Texas. The largest gains occurred in Oregon, Arizona, Georgia, Michigan, and Indiana. 4.0% of the population has access to only one HVS.
CONCLUSIONS: The incidence of CEA and the number of HVS has declined since 2012, converging fewer procedures onto a decreasing number of surgeons. Despite this, a majority of the U.S. population is within a 1-hour drive to an HVS. In some states, driving time to an HVS for CEA exceeds 3-6 hours. Though regionalizing surgical care correlates with improved outcomes, the potential burden on patient accessibility and satisfaction must be considered. 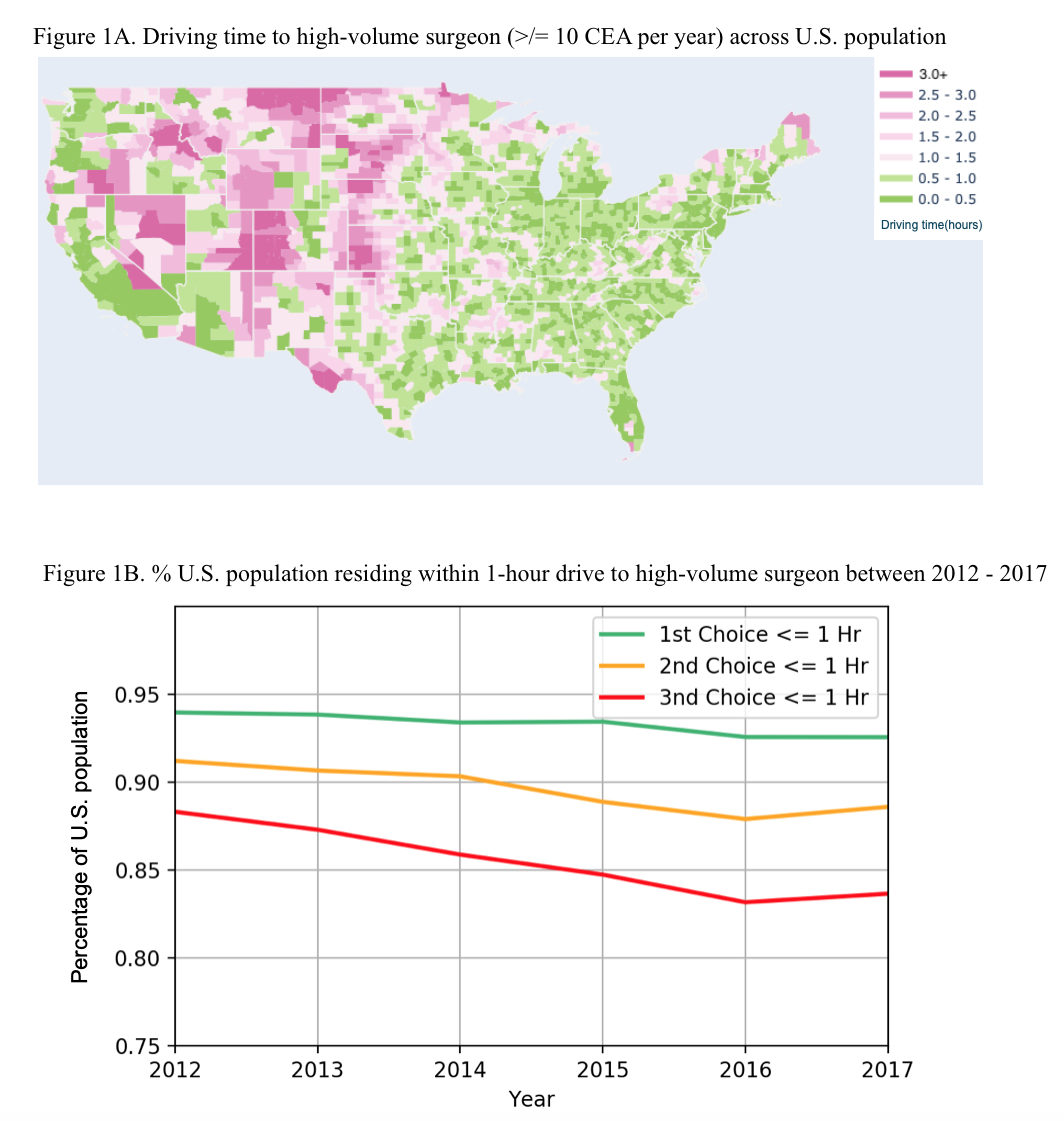
Back to 2020 ePosters
