Patients With Liver Disease Have Increased Mortality And Major Morbidities Following Infra-inguinal Bypass, But Not Following Endovascular Intervention
Sara L. Zettervall, MD, Kirsten Dansey, MD, Peter Soden, MD, Marc Schermerhorn, MD.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES: Liver disease has been shown to increase mortality following abdominal surgery including EVAR. However, the effect of liver disease on perioperative mortality following endovascular and open management of peripheral arterial disease has not been widely evaluated.
METHODS: The National Surgical Quality Improvement Program (NSQIP) was used to evaluate patients undergoing infra-inguinal bypass and endovascular intervention from 2005-2016. APRI score (AST to platelet ratio) is a sensitive, non-invasive tool recommended by the World Health Organization to identify significant liver fibrosis and was calculated for all patients. A value greater than 0.5 was used to identify patients with liver fibrosis. Demographics, comorbidities, and 30-day outcomes were compared for patients undergoing open and endovascular interventions among patients with and without liver fibrosis. A subgroup analysis was completed among patients with liver disease to compare open and endovascular outcomes. Multivariable regression was used to account for differences in baseline factors.
RESULTS: 17,603 patients underwent infra-inguinal bypasses including 15,932 (91%) without and 1671 (9%) with liver disease. Liver fibrosis was associated with higher mortality (3.8% vs. 2.4%, P<.01), major complications (23% vs. 20%, P=0.02), pulmonary complications (5.1% vs. 2.9%, P<.01), and renal complications (1.9% vs. 1.1%, P<.01) among patients undergoing bypass. These differences persisted following multivariable adjustment (Table). 7,830 patients underwent endovascular intervention including 6996 (89%) without and 836 (11%) with liver fibrosis. Liver fibrosis was also associated with higher mortality (4.7% vs. 2.2%, P<.01), pulmonary complications (3.9% vs. 2.5%, P =0.02), and renal complications (1.9% vs. 0.8%, P <.01) following endovascular intervention. After adjustment, only renal complications were higher among patients with liver fibrosis. When bypass was compared to endovascular intervention among patients with liver fibrosis, bypass was associated with a higher risk of mortality (OR: 2.7, 95% CI: 1.2-6.1) major complications (OR: 1.9 95% CI: 1.2-3.0), and pulmonary complications (OR: 3.1, 95% CI: 1.3-7.4) as compared to endovascular intervention.
CONCLUSIONS: Liver fibrosis was associated with significantly higher 30-day mortality and major complications following infra-inguinal bypass. Given the high rates of adverse events, surgeons should consider an endovascular first approach in managing peripheral arterial disease among those with liver disease. 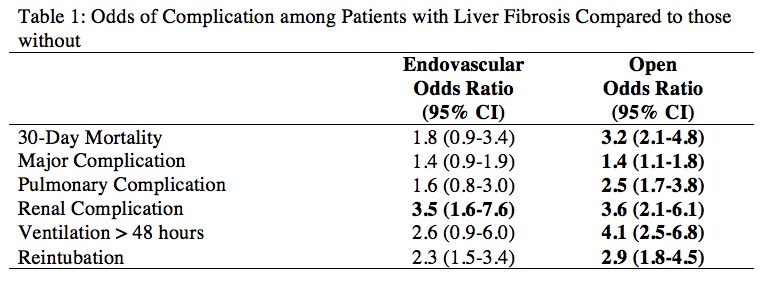
Back to 2020 ePosters
