Symptomatic Iliocaval and Extensive Left Lower Extremity DVT in COVID-19 Patient: A Case Report
Clinton Timmerman, OMS-IV, Arthelma C. Tyson, MD
AtlantiCare Regional Medical Center, Atlantic City, NJ
DEMOGRAPHICS: 60-year-old Caucasian female with medical history of controlled hypertension
HISTORY: A 60-year-old female presented to the emergency department with progressive left lower extremity swelling. Her presentation followed 3 weeks of bedrest in self-quarantine due to symptoms of fevers and mild cough. Imaging demonstrated occlusive left iliac vein thrombus with extension into the IVC. Chest X-ray demonstrated bilateral pulmonary infiltrates. Laboratory testing confirmed COVID-19 positivity.
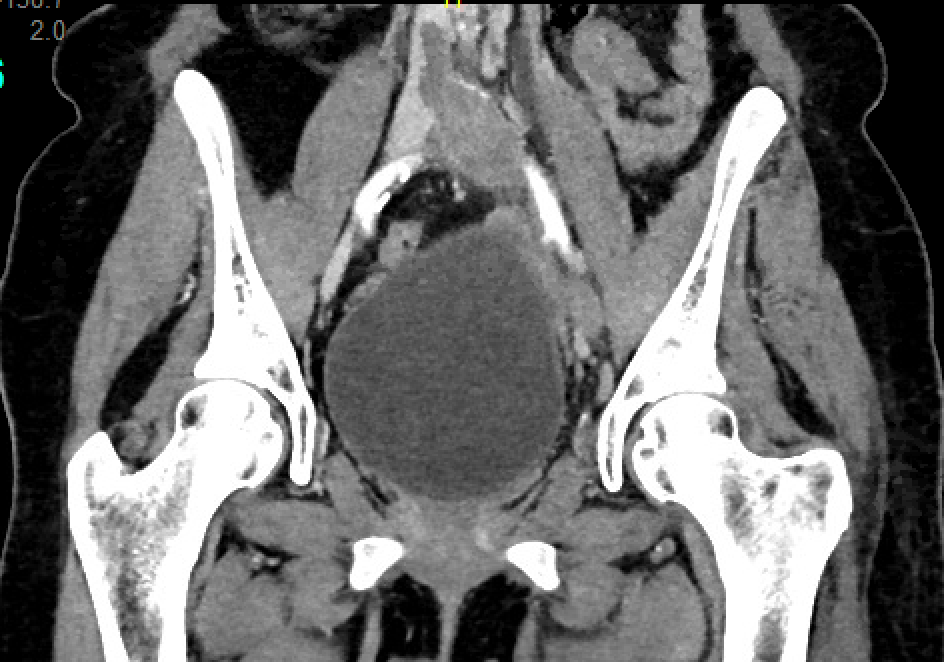
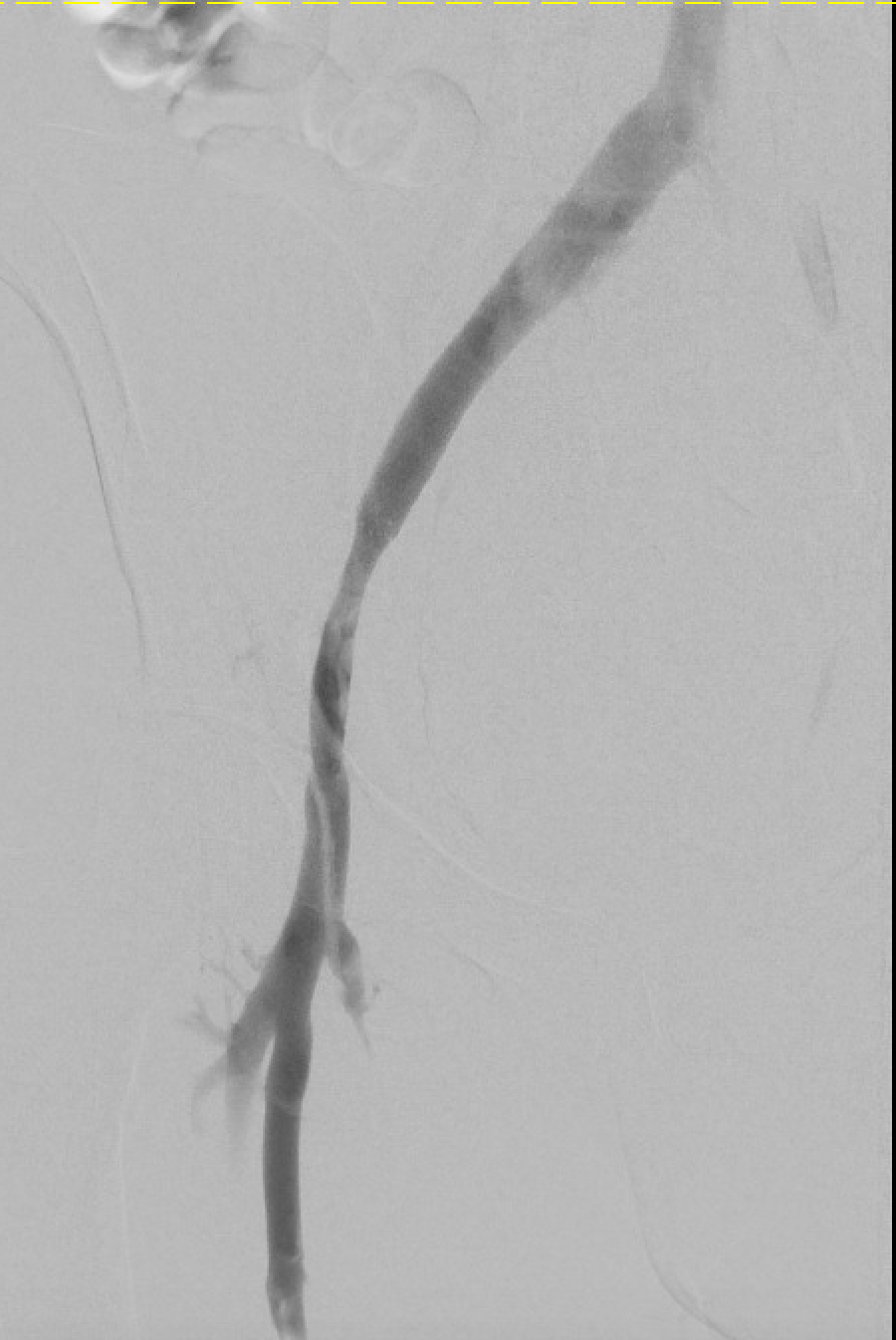
PLAN: She underwent retrievable IVC filter placement and overnight thrombolysis of the left iliac vein to IVC. On second-day intervention, she underwent thrombectomy and intravascular ultrasound (IVUS). Extrinsic left common iliac vein compression was identified, consistent with May-Thurner Syndrome. Her left common iliac vein was stented with no residual stenosis. Her swelling resolved. After 3 months of anticoagulation, she received a venogram and IVUS. IVUS demonstrated recurrent stenosis of the external iliac vein along with chronic nonocclusive thrombus and perivenous fibrosis. The external iliac vein was stented with good transition into the common iliac vein stent, and her IVC filter was retrieved.
DISCUSSION: This patient's COVID symptoms were mild, including dry cough and fevers. Nonetheless, she presented with significant thrombus. This was likely secondary to COVID-related hypercoagulability and decreased activity in the setting of outflow stenosis. Her left lower extremity symptoms fully resolved, and she has recovered from COVID infection. DVT risk factors include Virchow's Triad of stasis, hypercoagulability, and endothelial injury. The COVID-19 pandemic directly or indirectly contributes to these three factors, thereby increasing thrombosis risk. Data suggest increased hypercoagulability in patients with COVID-19 infection. Theories include but are not limited to cytokine storm and endothelial injury. Interestingly, increased thrombosis risk in COVID-19 patients occurs independent of the severity of systemic illness. The COVID-19 pandemic has posed innumerable challenges to the healthcare system. Additional studies and reports are required for further understanding of the multisystem effects of COVID-19 and its impact on the vascular system
Back to 2021 Abstracts
