Trans-septal Tevar For A 10-cm Dissecting Thoracoabdominal Aortic Aneurysm
Julia F. Chen, Prashanth Vallabhajosyula, Naiem Nassiri
Yale New Haven Hospital, New Haven, CT, USA
DEMOGRAPHICS: This is a 49-year-old female smoker with history of hypertension, CAD, CABG, renal cell carcinoma, nephrectomy, ESRD on hemodialysis, and stroke with residual left lower extremity paralysis. HISTORY: The patient previously underwent ascending aortic replacement for acute type A dissection 14 years prior. She presented with residual dissection of the arch and entire thoracoabdominal aorta with aneurysmal degeneration measuring 10-cm in maximum diameter (Figure A). CTA also demonstrated complete occlusion of the right external iliac artery and a left iliofemoral system supplied by the false lumen. PLAN: Following cervical debranching and carotid-subclavian bypass, the patient underwent elective TEVAR for her TBAD (3,10). A lumbar drain was placed, and continuous neuromonitoring (SSEP, EEG) was initiated. The left common femoral artery, known to be supplied by the false lumen, was accessed via micropuncture technique. A wire and catheter were passed into the false lumen of the abdominal aorta. Flush abdominal aortography demonstrated several large fenestrations (Figure B). Under roadmap guidance, the proximal-most fenestration was crossed using an angled Glidewire and a Berenstein catheter, allowing access into the true lumen, confirmed via angiography (Figure C). Serial dilation of the fenestration up to 18-french allowed insertion of a 20-french Gore DrySeal sheath with the tip positioned through the fenestration into the true lumen. Through this, a Lunderquist wire was positioned in the ascending aorta, and a buddy wire was inserted to allow for positioning of a pigtail catheter given the occluded contralateral iliofemoral system. A Medtronic Navion 34x34x223 was deployed just past the take-off of the debranched vessels followed by a 34x34x223 distal extension which was landed at the level of the celiac trunk. Balloon angioplasty of all seal and overlap sites was performed. Completion angiography demonstrated immediate augmentation of the true lumen with patent cervical and visceral vessels (Figure E). DISCUSSION:
Hybrid repair in patients with mega-aorta syndrome has previously been described only in the context of transfemoral true lumen access. We have presented here a strategy to proceed with endovascular repair in a patient with one occluded iliofemoral system and the other supplied entirely by the false lumen. 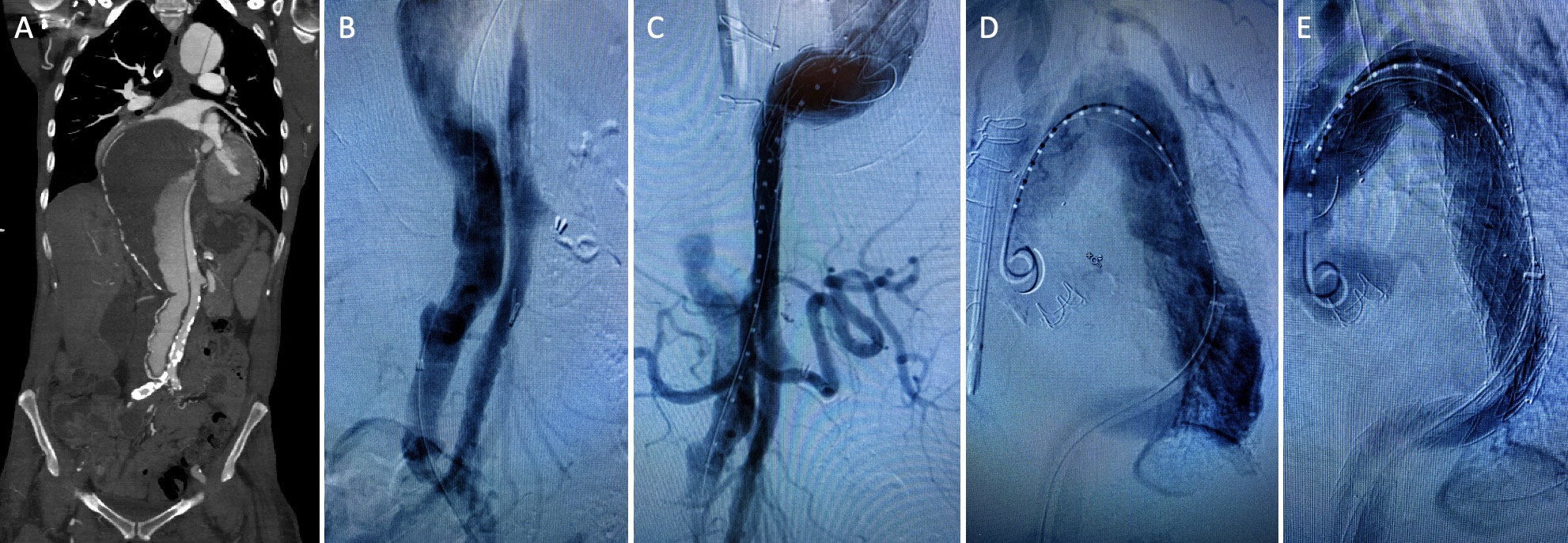
Back to 2021 Abstracts
