Zone 1 TEVAR Followed By Retrograde In-situ Laser Fenestration For Supra-aortic Branches For Ruptured Acute Type B Aortic Dissection Is A Feasible Option
Thekla Bacharach, MBBS, Anand Dayama, MD, Justin M. Milligan, MD, Jean M. Panneton, MD, FACS
EVMS, Norfolk, VA, USA
DEMOGRAPHICS: A 54-year-old healthy man presented with acute Type B Aortic Dissection (aTBAD)
HISTORY: The patient presented with acute onset severe back pain associated with left arm paresthesias. Computed tomography angiography (CTA) demonstrated an aTBAD with a tear at the left subclavian artery (LSA). Dissection extended retrograde to the origin of the left common carotid artery (LCCA). The descending thoracic aorta (DTA) measured 5 cm and an aberrant diminutive left vertebral artery (LVA) originated from the aortic arch with an aneurysmal origin.
PLAN: He was admitted for anti-impulse therapy with a plan for staged hemiarch debranching and Zone 1 TEVAR with LVA embolization in the sub-acute state. Two days later, he developed acute respiratory failure requiring intubation, and repeat CTA revealed a rapidly enlarging DTA, now 5.7 cm. He was emergently taken for hybrid hemiarch debranching and Zone 1 TEVAR. After supraclavicular exposure of the LCCA and LSCA, he became hypotensive SBP 50-60, with concern for rupture. The decision was made to proceed with TEVAR before completing debranching. The LVA was coil embolized and a Medtronic Navion CS 31 x 31 x 223 mm was then deployed in Zone 1 via percutaneous access. Then the L CCA was accessed for retrograde laser fenestration and a 10 mm x 39 mm iCAST stent was placed in the LCCA through the fenestration. The TEVAR was then extended distally with Medtronic Navion CS 34 x 34 x 182 mm.The LSA origin was embolized and a left carotid to subclavian artery bypass was performed with a 7 mm propaten graft. He was discharged on POD#7 after an uneventful recovery. One month surveillance CTA showed no endoleak, positive remodeling of the DTA (diameter 3.5 cm), patent left CCA stent and L CCA to LSA bypass.
DISCUSSION: This case illustrates the successful use of a retrograde in-situ laser fenestration technique for LCCA revascularization in a patient with a ruptured acute TBAD. The retrograde in-situ laser fenestration technique is an excellent alternative to the chimney/snorkel technique for rapid revascularization of the supra-aortic branches during emergent Zone 0/1 TEVAR in the absence of approved thoracic branched devices 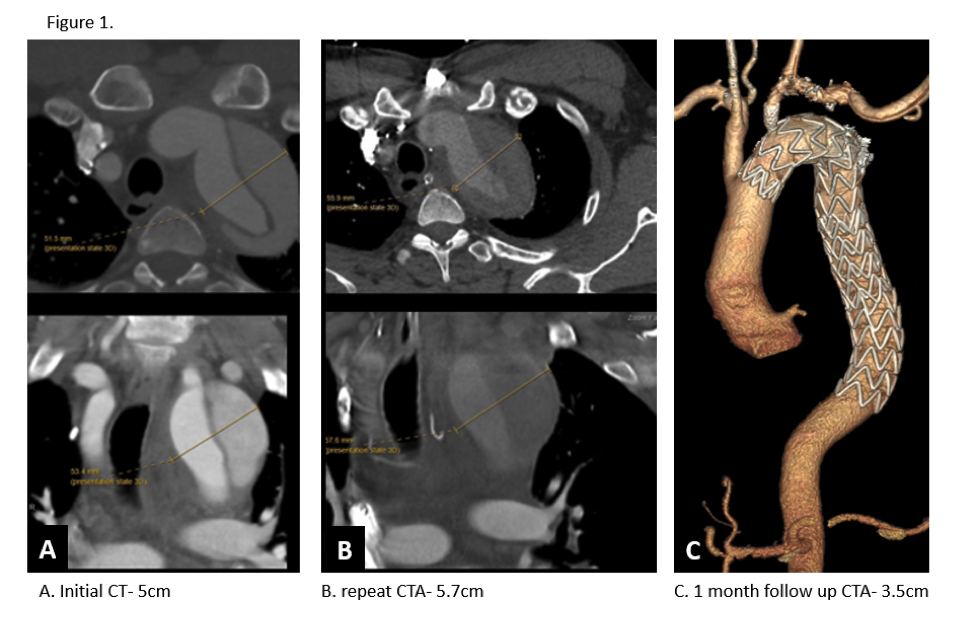
Back to 2021 Abstracts
