Aortoiliac And Open Revascularizations Are Protective Against Failure In Intermittent Claudicants Undergoing Intervention
Vashisht Madabhushi, M.D., Daniel Davenport, Ph.D, MBA, Stuart Jones, B.S., Sami Abul Khoudoud, B.S., Nathan Orr, M.D., David Minion, M.D., Eric Endean, M.D., Sam Tyagi, M.D..
University of Kentucky, Lexington, KY, USA.
OBJECTIVE: Intermittent claudication (IC), defined as reproducible leg pain with ambulation, is the most common symptomatic presentation of PAD. Despite the proven benefits of medical management, invasive revascularization of IC patients has experienced rapid growth. Revascularizations in IC patients are associated with increased rates of CLTI and amputation. The purpose of this study is to investigate outcomes of revascularization of IC patients based on treatment modality and region. This study aims to identify the outcomes of revascularizations of the aortoiliac (AI) versus infrainguinal (II) regions in patients with IC.
METHODS: This IRB-approved, single institute retrospective study reviewed all patients with an initial diagnosis of IC, who underwent revascularizations between 6/11/2003 to 4/24/2019. Patients were grouped based on the region of revascularization (AI or II) and procedure type (open or endovascular). Revascularization failure was defined as amputation or repeat revascularizations of the ipsilateral extremity at the same anatomic region. Primary outcomes were time to re-intervention and time to amputation after primary revascularization. Demographic data was analyzed using descriptive statistics. Kaplan Meir and multivariate analyses were performed comparing between anatomic regions and procedure types.
RESULTS: 341 patients underwent revascularizations for IC. The mean age was 60.3 years and 132 (38.7%) were female. Average follow-up time was 3.5 years. Of the AI procedures, 148 (79%) were endovascular, with a failure rate of 29.1% and 40 (21%) were open, with a failure rate of 32.5%. Of the 219 II revascularization procedures performed, 113 (52%) were endovascular procedures, with a failure rate of 46.0% and 106 (49%) were open procedures, with a failure rate of 50.9%. II revascularizations had higher rates of failure than AI revascularizations (p=0.027). There was no difference in rates of failure between open and endovascular revascularizations. (Figure 1) Multivariate analysis adjusting for age showed that AI region (HR: 0.5; 95% CI: 0.3 - 0.8) and open approach (HR: 0.5; 95% CI: 0.3 - 0.9) were independent protective factors against revascularization failure.
CONCLUSIONS: To the greatest possible extent, patients with IC should be medically managed. If revascularization is required, revascularizations of the AI region and open revascularizations have superior long-term outcomes. 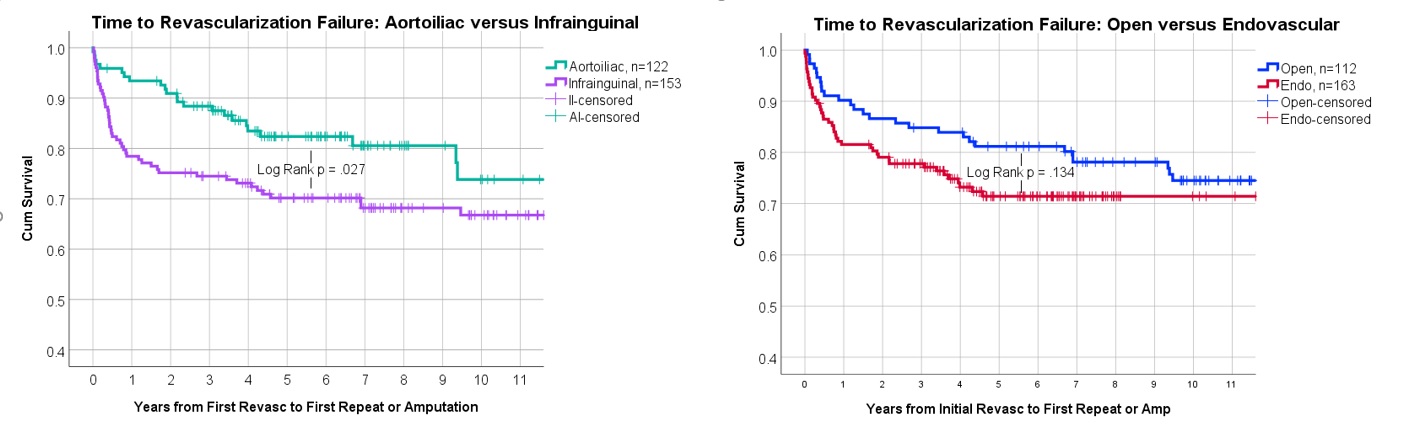
Back to 2021 Karmody Posters
