Association Of Perioperative Transfusions With Adverse Events After Infrainguinal Revascularization
Zachary A. Matthay, MD1, Eric J. Smith, BA1, Colleen P. Flanagan, MD1, Bian Wu, MD1, Mahmoud B. Malas, MD MHS2, Jade S. Hiramoto, MD1, Michael S. Conte, MD1, James C. Iannuzzi, MD MPH1.
1University of California, San Francisco, San Francisco, CA, USA, 2University of California, San Diego, San Diego, CA, USA.
Introduction
Patients with peripheral artery disease are at high risk for cardiovascular complications and death perioperatively. While transfusion of red blood cells (pRBCs) is associated with adverse events in patients undergoing revascularization, the role of transfusion timing and the risks associated with platelets and plasma remain incompletely understood. We aimed to further characterize the impact of transfusions on the risk of cardiovascular events after infrainguinal revascularization, hypothesizing that early transfusions and transfusion of ≥2pRBCs would be most associated with adverse events.
Methods
A single-center retrospective study was performed including 446 patients undergoing open (n=129) or endovascular (n=317) infrainguinal revascularization (2016-2019). Bivariate analyses compared demographics and outcomes by transfusion status. Multivariable logistic regression tested the associations of transfusions (pRBCs, platelets, and plasma [FFP]) with composite outcomes at 30 days: 1) Postoperative myocardial infarction (MI), congestive heart failure (CHF), or dysrhythmia, and 2) Major adverse cardiovascular events (MACE-postoperative MI, stroke or death).
Results
Of 446 patients, 18% received any transfusion intraoperatively or within 24 hours (17% pRBCs, 4% FFP, 3% platelets), and 14% received ≥2pRBCs within 48 hours. Patients transfused on POD-0 were older with higher rates of coronary artery disease and lower hemoglobin (all p<0.05). Rates of transfusion on POD-0 were 39% for patients undergoing open versus 7% for endovascular procedures (p<0.01) and 21% for patients with chronic limb threatening ischemia versus 14% for those with claudication (p=0.08). Transfusion on POD-0 was associated with MI (11% vs 2%, p<0.01), dysrhythmia (7% vs 1%, p<0.01), and MACE (16% vs 5%, p<0.01), and showed a trend for increased CHF (4% vs 2%, p=0.25) and mortality (6% vs 3%, p=0.13). In multivariable logistic regression, patients transfused on POD-0 and those receiving ≥2pRBCs within 48h had significantly increased odds of cardiovascular events (all p<0.05, Table). Transfusion of platelets and FFP showed similar trends, significant for the association of FFP transfusion with MACE (p=0.01, Table).
Conclusion
Perioperative transfusions are strongly associated with worse cardiovascular outcomes after infrainguinal revascularization. These findings may have prognostic value for identifying patients at higher risk for complications. However, prospective studies are needed to elucidate whether optimizing transfusion strategies mitigates these risks. 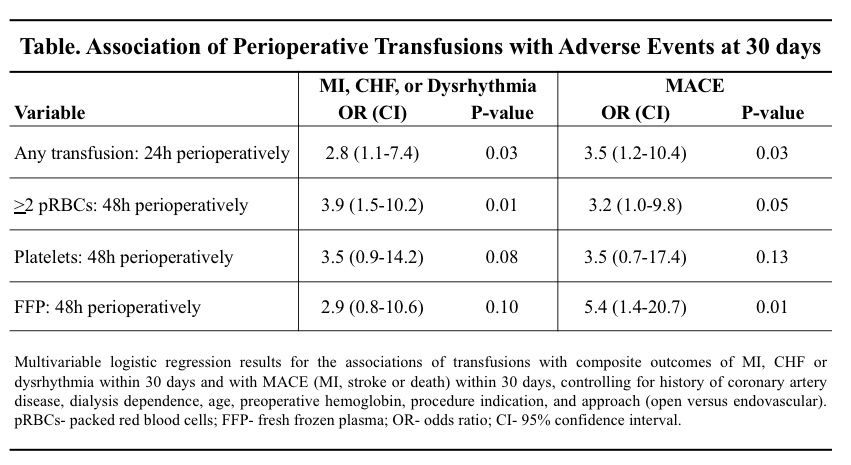
Back to 2021 Karmody Posters
