Improved Perioperative And Long-term Outcomes Of Carotid Endarterectomy In Dialysis Patients
Othman Mohamed-Asem Abdul-Malak, MD1, Theodore H. Yuo, MD2, Mohammad H. Eslami, MD1, Edith Tzeng, MD1, Nathan L. Liang, MD1.
1UPMC, pittsburgh, PA, USA, 2UPMC, Pittsburgh, PA, USA.
OBJECTIVES: Prior studies have shown poor perioperative and long-term survival of patients on dialysis (HD) undergoing carotid endarterectomy (CEA). Identifying patients likely to have acceptable perioperative and long-term outcomes will allow providers to select HD patients that may survive long enough in the post-operative period to benefit from carotid revascularization.
METHODS: We queried the Vascular Quality Initiative CEA dataset from 2003-2020. Patients with missing dialysis or death status or undergoing concomitant coronary artery bypass were excluded. Demographics, co-morbidities, procedural details and outcomes were collected. Standard statistical methods were utilized.
RESULTS: We identified 124,266 patients undergoing CEA with 1281 (1.1%) on HD. Compared to non-HD patients, HD patients were younger (68.7 vs 70.5 years, p<0.001), more likely to have common preoperative comorbidities (CAD 43.8% vs 26.7%, p<0.001; CHF 38.9% vs 11.2%, p<0.001; pre-op anemia 27.1% vs 4.5%, p<0.001), live in skilled nursing facilities (3.4% vs 1.2%, p<0.001), have prior lower extremity arterial intervention (bypass 12.5% vs 5.6%, p<0.001; endovascular 20.8% vs 8.9%, p<0.001), and are less ambulatory (70.6% vs 89.6%, p<0.001). HD patients had higher rates of 30-day mortality (2.4% vs 0.6%, p<0.001), and postoperative MI (1.5% vs 0.7%, p<0.001), but no difference in 30-day postoperative stroke (0.23% vs 0.48%, p=0.206). Within the HD cohort 28.5% (N=366) were symptomatic in the prior 6 months; there was no difference in rate of 30-day postoperative stroke between symptomatic (0.55%) vs asymptomatic (0.11%, p=0.144) or 30-day mortality (3.01% vs 2.19%, p=0.388). The HD cohort had a 1-year survival of 85% and a 5-year survival of 63% (Figure 1), there was no difference in survival when stratified by symptomatic status (p=0.644). On adjusted Cox analysis, prior lower extremity bypass (HR 1.63,[1.19,2.22],p=0.002), pre-op anemia (HR 1.41,[1.09,1.81],p=0.008), non-ambulatory status (HR 1.34,[1.13,1.61],p=0.001), increasing age (HR 1.22,[1.06,1.3],p=0.004), pre-operative current smoking (HR 1.25,[1.03,1.3],p=0.006), and history of CHF (HR 1.15,[1.15,1.3],p=0.026) were independently associated with long-term mortality.CONCLUSIONS: HD patients have lower combined postop stroke and death rates than previously reported after CEA. Decreasing ambulatory status and the absence of significant cardiac or peripheral arterial disease may be useful for identifying HD patients who may benefit from CEA. 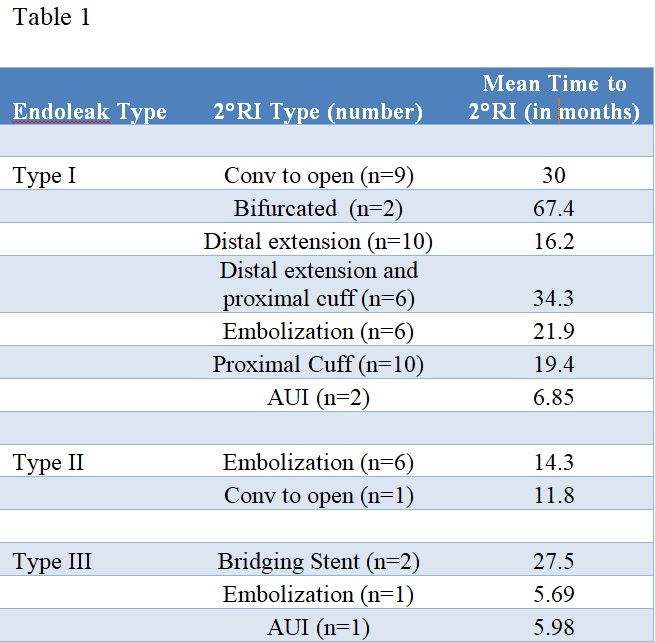
Back to 2021 Karmody Posters
