Establishing And Maintaining A Remote Vascular Surgery Aortic Program: A Single-center Five-year Experience
Joshua P. Kronenfeld, MD, Naixin Kang, MD, Alberto Lopez, MD, Stefan Kenel-Pierre, MD, Jorge Rey, MD, Arash Bornak, MD.
University of Miami Miller School of Medicine & Miami VAMC, Miami, FL, USA.
OBJECTIVES: Telehealth has been utilized to deliver remote care to patients for many years, and 76% of hospital systems have an established telehealth system. The use of telehealth by surgeons poses unique challenges including preoperative physical examination and postoperative wound management. While these challenges exist, a regional Veterans Administration Hospital (VA) established a telehealth program to provide advanced aortic surgery for patients located in remote areas throughout the state. The objective of this study is to detail the process of establishing a vascular surgery aortic telehealth program and to report the outcomes of a five-year experience.
METHODS: A telehealth program was established between two regional VA hospitals, one of which was without a comprehensive aortic surgical program, until such program was established at the referring institution. A retrospective review was performed of all patients who underwent aortic surgery between 2014 and 2019. Operative data, demographics, perioperative complications, and follow-up data were reviewed.
RESULTS: Between 2014-2019 a total of 109 patients underwent aortic surgery for occlusive disease and aneurysms at the VA hospital. They evaluated pre-operatively and followed remotely via telehealth. Median age was 68, 107 (98.2%) were male. 28 (25.7%) underwent open aortic repair and 80 (74.3%) underwent an endovascular repair. 101 patients were followed for a median of 25.1 months, 7 (6.4%) lost follow-up or were non-compliant, and 1 (0.9%) changed state. While 41 (37.6%) patients encountered at least one complication throughout their postoperative course, only 8 (7.3%) required readmission. Most of these complications were managed remotely via telehealth, but 2 (1.8%) patients required transfer back to the operative VA for additional care.
CONCLUSIONS: Telemedicine is a great tool to provide perioperative care and long-term follow-up for aortic patients in remote locations. Post-operative care and complications are manageable from distance, and patient compliance for long-term follow-up, including monitoring imaging, is excellent. 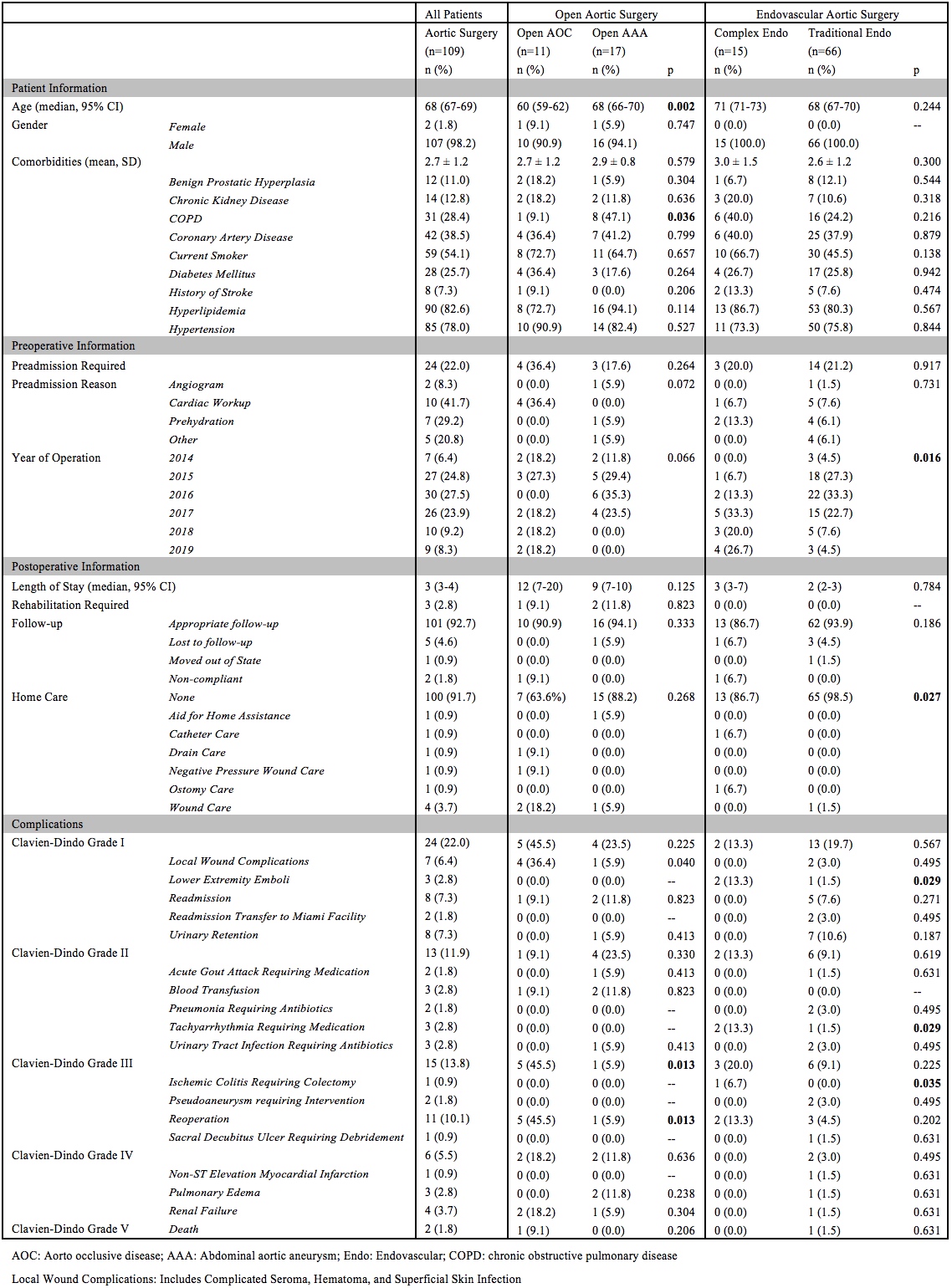
Back to 2021 Karmody Posters
