Temporary Diaphragm Pacing For Patients At Risk Of Prolonged Mechanical Ventilation After Thoracoabdominal Aortic Aneurysm Repair
Aric A. Wogsland, MD, Saideep Bose, MD, Norman H. Kumins, MD, Benjamin D. Colvard, MD, Vikram S. Kashyap, MD, Raymond P. Onders, MD, Jae S. Cho, MD.
Case Western Reserve University School of Medicine, Cleveland, OH, USA.
Objectives: Prolonged mechanical ventilation (PMV, ventilator support >72 hours) after thoracoabdominal aortic aneurysm (TAAA) surgery is common, with the incidence rate of >50%. Prior studies in other patient populations have demonstrated that diaphragm pacing (DP) overcomes ventilator induced diaphragm dysfunction (VIDD) and improves pulmonary function in patients with unilateral diaphragm paralysis. The goal of this study was to determine if this novel technology may be applicable to TAAA repair.
Methods:Four patients with high risk for PMV after open TAAA repair between June and August 2020 who underwent implantation of an FDA-authorized temporary diaphragm pacing system were reviewed. All patients underwent thoracoabdominal exposure with circumferential division of the diaphragm with preservation of the phrenic nerve. After aortic repair, the diaphragm was approximated in the usual fashion and two electrodes were placed in the diaphragm lateral and inferior to the phrenic nerve and the wires tunneled percutaneously. Post-operatively, the DP stimulation was instituted to prevent atrophy and VIDD. The diaphragm electromyography (dEMG) was analyzed prior to DP and daily. Key clinical outcome variables were recorded.
Results:All 4 patients (3 males, mean age 73 years [range, 60-81]) underwent urgent or emergency repair utilizing left heart bypass with a heart-lung machine. Indications were rupture (2) and symptomatic (2, one of which was mycotic) TAAA. In 1 patient with rupture, elective repair had been deferred due to known compromised baseline pulmonary status. In 2 patients adequate pulmonary function evaluation could not be obtained due to the urgency of the operation. All 4 were former smokers, 3 of whom had chronic obstructive pulmonary disease. Median total ventilation time including operating time was 23 hours (range, 16-30.5). Median post-operative mechanical ventilation time was 13.5 hours (range, 8-17.5). In all patients significant improvement in dEMG was noted with DP (Figure). There were no re-intubations. One patient required high flow nasal cannula for 29 hours after extubation. DP lasted 2-4 days (median 2.75 days) with subsequent removal without any complications.
Conclusion:Diaphragm Pacing may be an effective way to mitigate PMV and VIDD after TAAA repair. A further comparative study is warranted. 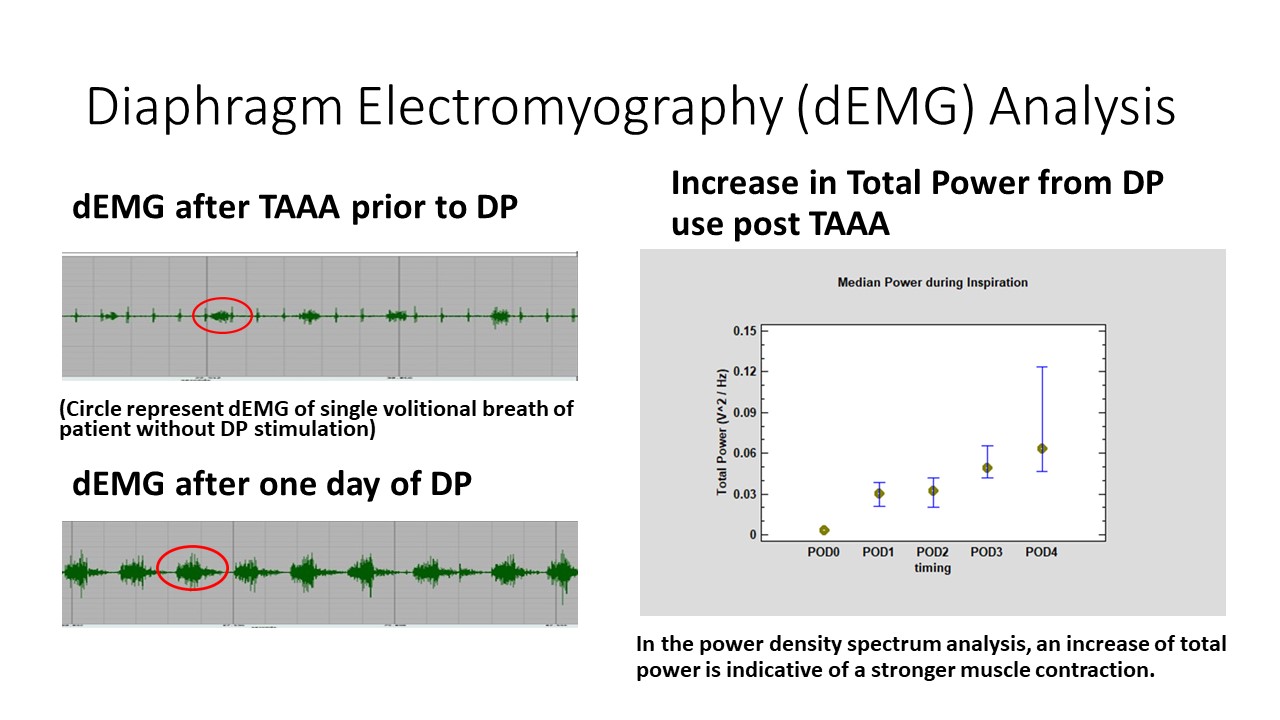
Back to 2021 Karmody Posters
