NAC Treatment After Lower Extremity Amputation Improves Areas Of Perfusion Defect And Wound Healing Outcomes
Jin V. Lee, Connor Engel, Shirli Tay, MPHS, Kshitij Desai, MD, Gayan DeSilva, MD, Clay Semenkovich, MD, Mohamed Zayed, MD PhD.
Washington University School of Medicine, St. Louis, MO, USA.
OBJECTIVES - Patients with critical limb threatening ischemia (CLTI) and diabetes are at increased risk of poor major amputation site healing. Preclinical studies have demonstrated that the antioxidant N-acetyl-cysteine (NAC) can augment tissue perfusion and angiogenesis in mice. We hypothesize that peri-operative administration of NAC in patients with CLTI improves amputation stump perfusion and healing.
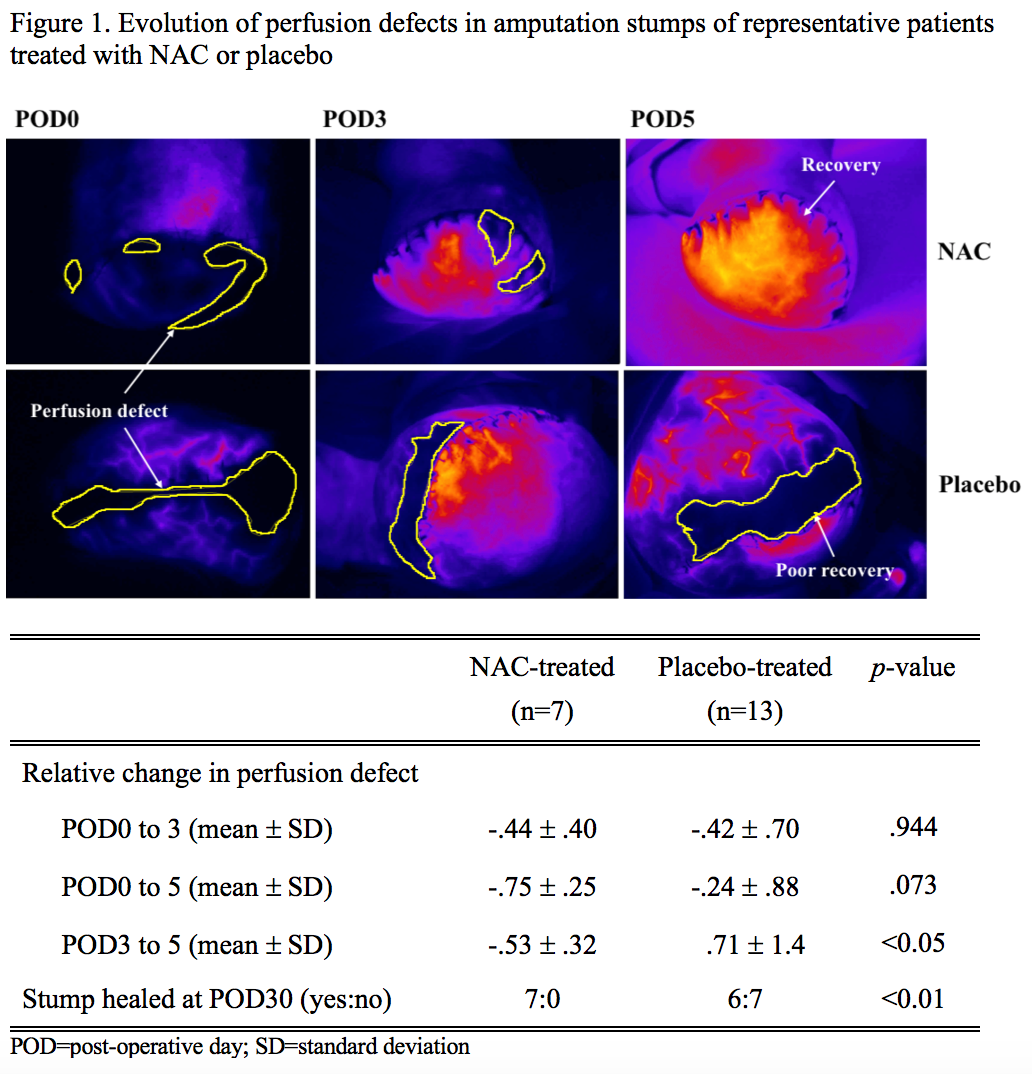
METHODS - In a randomized prospective, double-blinded, placebo-controlled, pilot clinical trial, patients with CTLI were recruited at the time of major lower extremity amputation. Patients were randomized to a 5-day peri-operative course of intravenous NAC or placebo treatment. Amputation stump perfusion was evaluated on post-operative day 0 (POD0), 3, and 5 using non-invasive Laser-Assisted Fluorescent Angiography (LAFA; SPY Elite®system). Rate of arterial inflow and peak perfusion were determined using dynamic intensity versus time analysis. Perfusion defects were determined at the time of peak perfusion as a percentage stump surface area (Figure1). Amputation stump healing was also evaluated on POD3, 5, and 30 using modified Bates-Jensen score. Continuous variables were analyzed using the Student’s t-test. Categorical variables were analyzed using Fisher’s exact test.
RESULTS - A total of 33 patients were enrolled in the study. One patient withdrew consent and 8 were excluded for missing/incomplete files. Four patients (3 NAC, 1 placebo) had no perfusion defects. In the remaining 20 patients (7 NAC, 13 placebo) with baseline perfusion defects, NAC-treated patients had a more favorable recovery slope compared to control. From POD3 to 5, NAC-treated patients had a greater relative reduction in defect size (-53% decrease vs. +71%; p<0.05; Table1), whereas perfusion defects increased in the placebo group. Patients that received NAC also had superior healing outcomes at POD30 (100% healing for NAC vs. 46% for placebo; p<0.01; Table1). No differences in LAFA-derived rate of arterial inflow or time to peak perfusion were observed between the study groups.
RESULTS - In patients with CLTI and amputation stump perfusion defects at baseline, peri-operative NAC administration may improve short-term perfusion and long-term tissue healing. Intraoperative LAFA may help identify patients with decreased stump perfusion who can benefit from early therapeutic intervention.
Back to 2021 Abstracts
