Traumatic Lower Extremity Vascular Injuries And Limb Salvage In A Civilian Urban Trauma Center
Eva Maria Urrechaga, MD1, Sinan Jabori2, Stefan Kenel-Pierre, MD1, Alberto J. Lopez, MD1, Naixin Kang, MD1, Rishi Rattan, MD3, Jorge Rey, MD1, Arash Bornak, MD1.
1Department of Surgery-Vascular & Endovascular Surgery, University of Miami & Ryder Trauma Center, Miami, FL, USA, 2University of Miami Miller School of Medicine, Miami, FL, USA, 3Department of Surgery-Trauma Surgery, University of Miami & Ryder Trauma Center, Miami, FL, USA.
OBJECTIVE: Data on management of traumatic lower extremity injuries comes largely from military experience, with few civilian centers captured. This study reports on the experience of an urban trauma center and factors associated with limb loss. METHODS: An academic urban level 1 trauma center was queried for lower extremity vascular injury between 2013-2020. Exclusions included immediate amputation, death in emergent OR, or no vascular intervention. Demographic and clinical variables were recorded. Primary outcome of interest was limb salvage. Secondary outcomes included mortality, mobility, and post-operative complications. RESULTS: 80 subjects were identified: 91% male, mean age 33±15yrs, 68% penetrating, and median ISS 13[9-18]. Revascularization was performed by vascular surgery in 60% and trauma in 40% with 3 trauma cases requiring intraoperative vascular consult for revascularization failure. Trauma more often utilized prosthetic interposition (28% vs 5%, p<0.001 and vascular more commonly performed below knee interventions (89% vs 12%, p<0.001). Associated fractures (51%) more often underwent bypass (p=0.036), interposition graft (p=0.007), and involved vascular surgery (p=0.014). Return to OR for complication occurred in 31%: compartment syndrome (14%), revascularization failure (10%), bleeding (3%), and wound complications (12%). Mortality was 5%, with 90% limb salvage among survivors. Factors associated with limb loss (Table) included female sex (p=0.003), blunt injury (p=0.001), associated fracture (p=0.005), significant soft tissue injury (p=0.006), bypass (p=0.004), and concomitant ortho procedure (p=0.003). Subjects requiring temporary vascular shunt had higher ISS than no shunt (21vs14, p=0.015), without difference in compartment syndrome, length of stay, secondary return to OR, limb loss, or mortality. 58 patients followed up in clinic for a median 36[14-110] days, with only 55% following up at >30 days. 41% reported ambulation without assistance, 16% neuromotor deficit, and only 1 subsequent amputation. 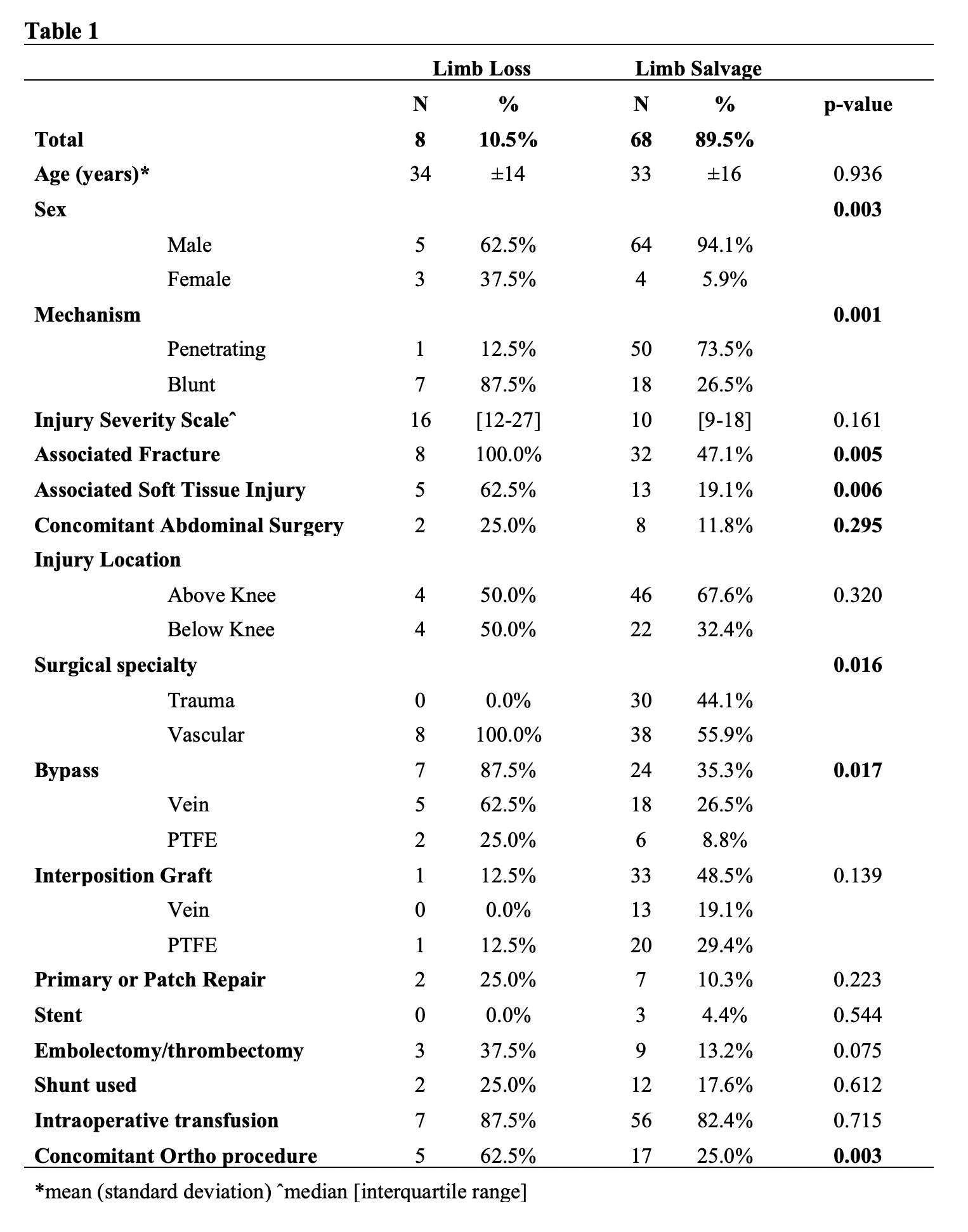 CONCLUSION: Extremities with fracture or extensive soft tissue injury often require more complex repair including distal bypass, necessitating the involvement of a vascular surgeon. In this group of patients, female with blunt trauma are particularly at risk of limb loss. Although early limb salvage in our cohort is high, mid and long-term repair latency and limb salvage cannot be accurately assessed due to lack of adequate clinic follow up.
CONCLUSION: Extremities with fracture or extensive soft tissue injury often require more complex repair including distal bypass, necessitating the involvement of a vascular surgeon. In this group of patients, female with blunt trauma are particularly at risk of limb loss. Although early limb salvage in our cohort is high, mid and long-term repair latency and limb salvage cannot be accurately assessed due to lack of adequate clinic follow up.
Back to 2021 Abstracts
