Effect Of Anticoagulation And Antiplatelet Medications On Aortic Remodeling After Thoracic Endovascular Aortic Repair For Type B Aortic Dissection
Heepeel Chang, MD1, Caron B. Rockman, MD1, Neal S. Cayne, MD1, Glenn R. Jacobowitz, MD1, Frank J. Veith, MD1, Virendra I. Patel, MD, MPH2, Karan Garg, MD1.
1NYU Langone Medical Center, New York, NY, USA, 2Columbia University Medical Center, New York, NY, USA.
OBJECTIVES: To date, few studies adequately evaluate the impact of anticoagulation and antiplatelet medications on aortic remodeling for type B thoracic dissection (TBAD) after thoracic endovascular aortic repair (TEVAR). As such, we assessed the relationship between chronic anticoagulation/antiplatelet medications and aortic remodeling of patients with TBAD after TEVAR.
METHODS: Records of the Vascular Quality Initiative TEVAR registry (2011-2019) were reviewed. Procedures performed for dissection-related pathology were included. Primary outcomes included complete false lumen thrombosis, reintervention-free survival and endoleak at 18-months. Primary outcomes were compared between patients with and without chronic anticoagulants (AC and non-AC). A subgroup analysis was performed to assess the effect of antiplatelet medications (none, single-antiplatelet and dual-antiplatelets) in the non-AC group. Cox proportional hazards models were used to estimate the effect of different antithrombotic therapies on primary outcomes.
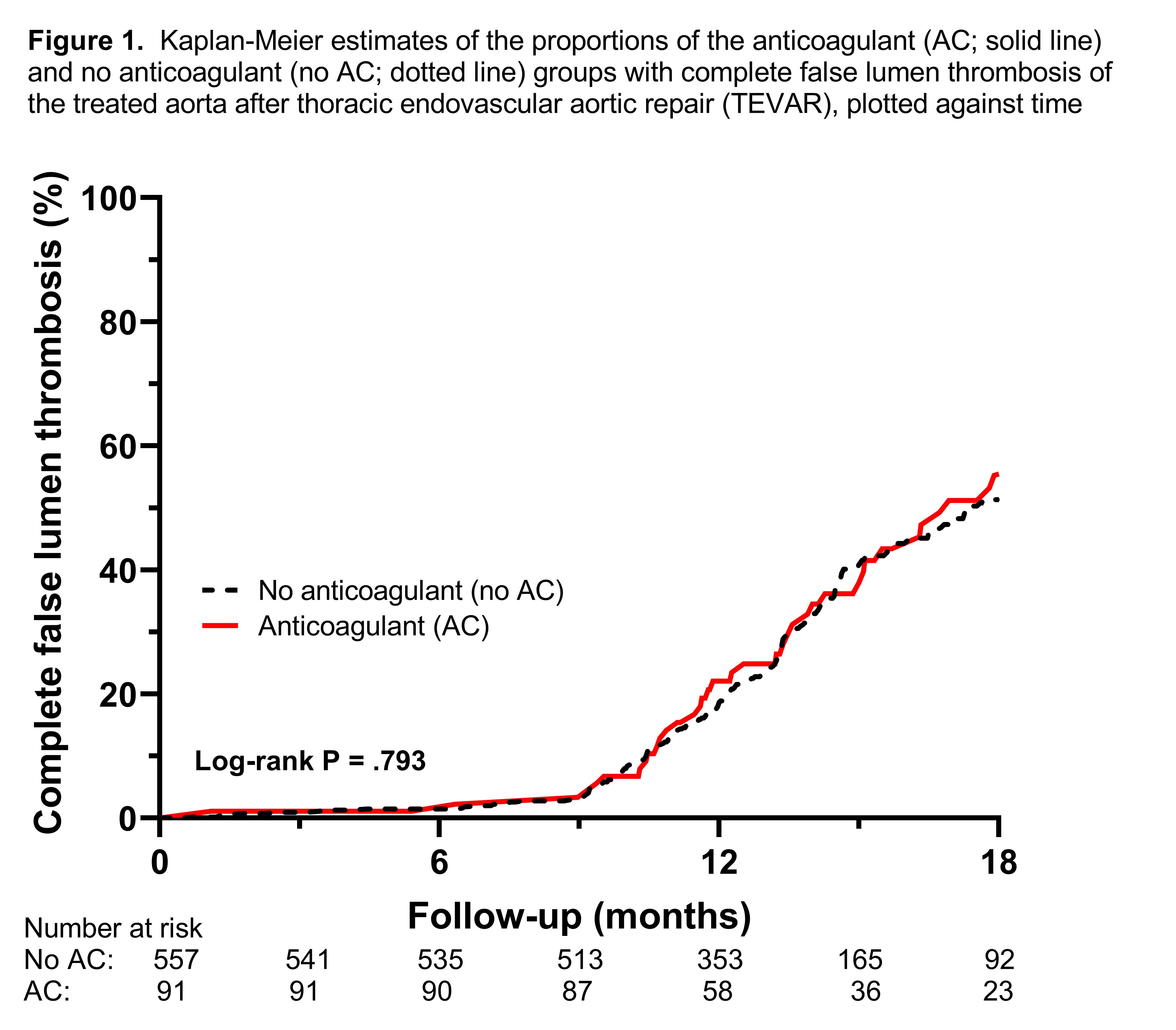
RESULTS: 1,507 patients (mean age, 60.7±12.2 years; male, 68.3%) were identified with a mean follow-up of 18.9±13.7 months. 201 (14%) patients were on anticoagulation therapy at follow-up. There were no differences in the mean preoperative thoracic aortic diameter or the number of endografts used. The status of false lumen thrombosis and endoleaks were available in 648 (43%) and 1,023 patients (68%), respectively. At 18 months, the rates of complete false lumen thrombosis (51.3% vs. 47.5%; P=.182), reinterventions (9% vs. 10.6% P=.175), all-cause mortality (97.6% vs. 96.9%; P=.561) and endoleaks (18.8% vs. 22%; P=.397) were similar in the AC and non-AC groups, respectively (Figure). Controlling for covariates with the Cox regression method, anticoagulant use was not independently associated with a decreased risk of complete false lumen thrombosis (hazard ratio, HR 0.79; 95% confidence interval, CI: 0.54-1.16; P=.235) or increased risks of reintervention (HR 1.06; 95% CI:0.9-1.24; P=.484) and endoleak (HR 0.97; 95% CI: 0.83-1.14; P=.725). Within the non-AC group, antiplatelet medications did not affect the rates of complete false lumen thrombosis, reintervention or endoleak.
CONCLUSIONS: The use of chronic anticoagulation and antiplatelet medications did not adversely affect the rate of complete false lumen thrombosis and positive aortic remodeling in patients who underwent TEVAR for TBAD. Anticoagulation and antiplatelet medications may be safely used in patients who undergo TEVAR for TBAD.
Back to 2021 Abstracts
