Risk Factors For Early Mortality With Inferior Vena Cava Filters
Anand Brahmandam, MBBS1, Valentyna Kostiuk, BS2, Scott Grubman, BS2, Eric Schneider, PhD3, Britt H. Tonnessen, MD1, Hamid Mojibian, MD4, Cassius Iyad Ochoa Chaar, MD1.
1Division of Vascular Surgery, Department of Surgery, Yale University School of Medicine, New Haven, CT, USA, 2Yale University School of Medicine, New Haven, CT, USA, 3Center for Health Services and Outcomes Research, Department of Surgery, Yale University School of Medicine, New Haven, CT, USA, 4Division of Interventional Radiology, Department of Radiology and Biomedical Imaging, Yale University School of Medicine, New Haven, CT, USA.
Objectives: Inferior Vena Cava filters (IVCF) placement is a low risk procedure. Yet, a significant number of patients expire within 30 days of insertion because of underlying disease. The benefit of IVCF placement in this group of patients is debatable. This study aims to assess the incidence and risk factors for early mortality after IVCF placement in a tertiary care center.
Methods: A retrospective review of consecutive patients undergoing IVCF placement between 2007 and 2019 was performed. Patients were divided into early-mortality group if they suffered 30-day mortality and survival group if they survived that period. Baseline characteristics and outcomes were compared. Temporal trends of early-mortality IVCF and prophylactic IVCF use was derived. All statistical analysis was performed using Stata.
Results: A total of 1,409 IVCF were placed during the study period. The 30-day mortality was 12% and those 173 patients constituted the early-mortality group. The use of early-mortality IVCF as well as prophylactic IVCF did not significantly change over the study period quartiles (figure). There was no mortality related to IVCF insertion in either group and no difference in hematoma formation, migration, fracture, or penetration between the 2 groups in the perioperative period. Patients in the survival group were more likely to undergo prophylactic IVCF placement (20.4% vs 6.9%, P=0.001). Interestingly, there was a higher rate of iliac vein (17.9% vs 11.1%; P<0.009) and femoral vein deep vein thrombosis (49.1% vs 39.9%, P=0.02) in the early-mortality group. Patients in the early-mortality group were more likely to have older age but there was no significant difference in gender. Patients with early-mortality after IVCF placement were significantly more likely to have cancer (59.7% vs 29.3%; P=0.001) and have failure of anticoagulation (10.59% vs 6.02%, P=0.024). Conversely, patients in the early-mortality group were significantly less likely to have trauma (4.8% vs 18.2%, P<0.01) or recent major surgery as risk factors (13.3% vs 27.3%; P=0.04).
Conclusion: There is a high 30-day mortality after IVCF placement in certain groups of patients. This study highlights the risk factors for early mortality with IVCF placement, in order to promote more effective utilization. 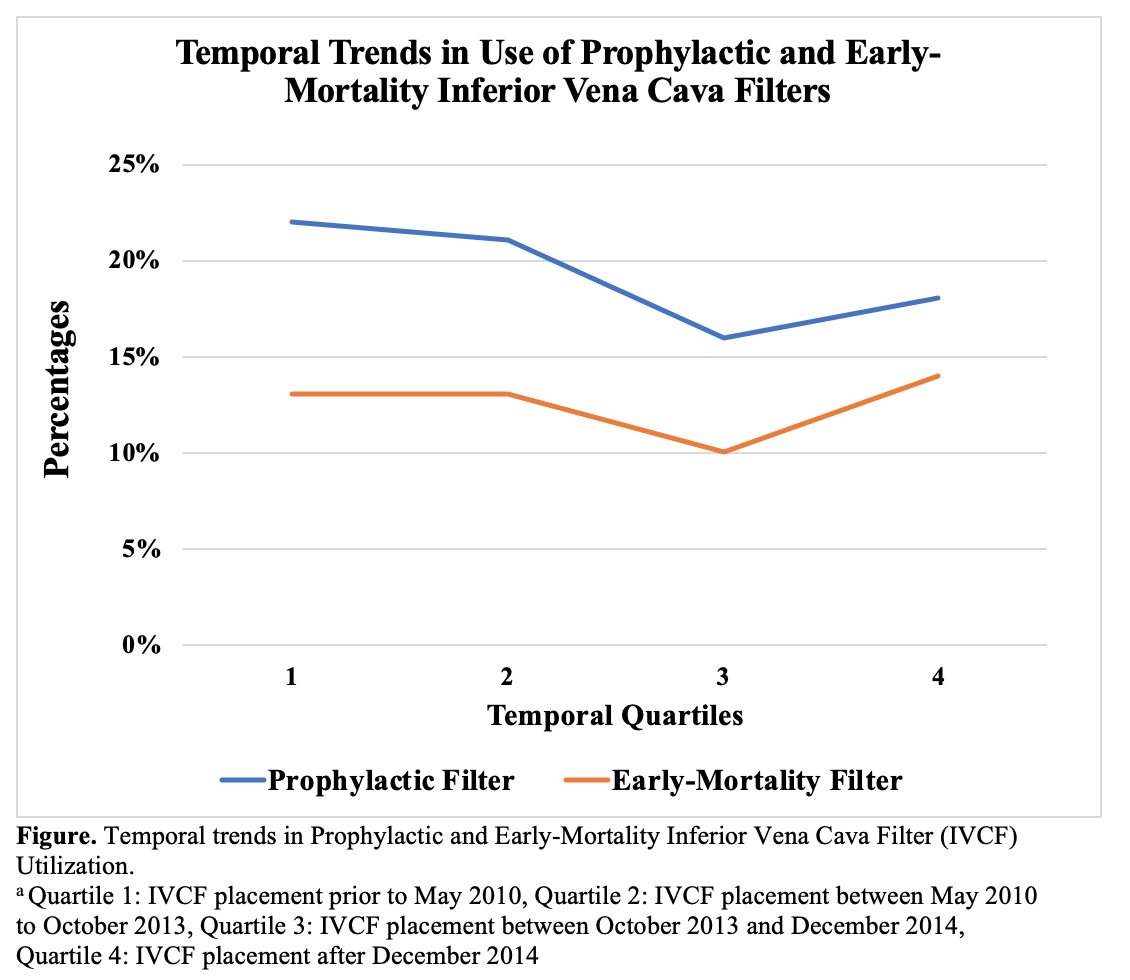
Back to 2021 Abstracts
