Venous Mesenteric Thrombosis Carries High Procedural Burden and Low Mortality in Patients With Benign Presentation
Zach M. Feldman, MD, Linda J. Wang, MD, MBA, Elizabeth L. Chou, MD, Matthew J. Eagleton, MD, Mark F. Conrad, MD, MMSc.
Massachusetts General Hospital, Boston, MA
OBJECTIVE
Venous mesenteric thrombosis (VMT) presents with variable severity resulting in a spectrum of outcomes. This study sought to characterize the natural history of VMT and identify factors associated with adverse outcomes.
METHODS
All patients who presented to our institution with VMT between 1993-2015 were identified. Images were reviewed to determine thrombosis location and charts were reviewed to identify clinical factors and outcomes. Univariate analysis was performed for demographics, comorbidities, and presenting characteristics, with primary outcomes of intervention, readmission, and 30-day mortality.
RESULTS
109 patients with VMT were identified. Locations of thrombosis were: superior mesenteric vein (SMV, 31.2%); SMV and portal vein (35.8%); SMV, portal, and splenic vein (15.6%); and other combinations of portomesenteric veins (17.4%), without correlation between location and outcomes. Most were male (60.6%), 35.8% were prescribed anticoagulation, and 21.1% were prescribed aspirin. Mean age was 61.3 years. Over half had hypercoagulable state (51.4%), 22.9% had prior bowel resection, 22.0% were active smokers, and 14.7% had prior mesenteric vessel intervention, including TIPS. 39 patients underwent 89 procedures during their hospitalization, while 26 patients underwent surgical intervention. Prior mesenteric vessel procedure, leukocytosis above 10K/uL, and lactatemia above 1.5mmol/L were associated with increased need for surgical intervention (p<0.05). Prior bowel resection trended toward increased intervention (p=0.10). However, symptoms under 2 weeks (p<0.05) and prescribed anticoagulation (p=0.07) were associated with decreased surgical intervention. Readmission was increased in patients with higher Charlson comorbidity scores (p=0.07) and weight loss (p=0.06). 30-day mortality was low in this cohort (6.4%). Abdominal tenderness and lactatemia were associated with increased 30-day mortality (6.8% versus 2.9%, p<0.05, and 15.0% versus 0%, p<0.05), although prior intervention did not confer mortality effect. Those with underlying hypercoagulable state had similar intervention rates (46.2% versus 54.3%, p=0.54) but increased 30-day mortality (8.9% versus 3.8%, p=0.48), although this did not reach statistical significance. Smokers trended toward worsened combined adverse outcomes (surgical intervention, 30-day readmission, 30-day mortality, p=0.07).
CONCLUSION
The 30-day mortality of VMT is low but over one-third of patients required intervention beyond anticoagulation. Comorbidity, prior mesenteric vessel or intestinal operation, and presentation with tenderness or relevant laboratory abnormalities portend worsened outcomes.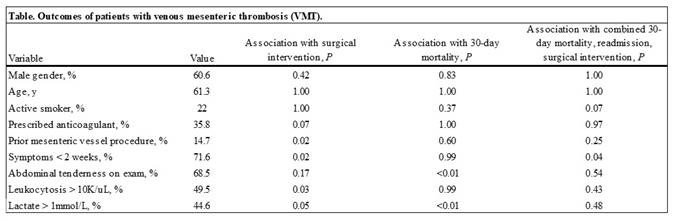
Back to 2021 Abstracts
