Shunt Intention During Eversion Carotid Endarterectomy And Perioperative Stroke Risk
Scott R. Levin, M.D., M.Sc.1, Alik Farber, M.D., M.B.A.1, Philip P. Goodney, M.D., M.S.2, Virendra I. Patel, M.D., M.P.H.3, Rebecca Hasley, M.D.1, Nkiruka Arinze, M.D.1, Thomas W. Cheng, M.S.1, Denis Rybin, Ph.D.1, Jeffrey J. Siracuse, M.D., M.B.A.1.
1Boston University, Boston, MA, USA, 2Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA, 3Columbia University Medical Center, New York, NY, USA.
OBJECTIVES: Shunting during eversion carotid endarterectomy (eCEA) may be technically challenging. Whether shunting practice patterns modify perioperative stroke risk after eCEA is unclear. We aimed to compare eCEA outcomes based on whether surgeons prospectively planned or planned not to shunt. Secondarily, we sought to compare outcomes based on shunting indication.
METHODS: The Vascular Quality Initiative (2011-2019) was queried for eCEAs. Univariable and multivariable analyses compared outcomes based on 1) whether surgeons planned or planned not to shunt and 2) whether shunting was routine practice, preoperatively indicated, intraoperatively indicated, or not performed (Figure).
RESULTS: Among 13,207 eCEAs, surgeons planned to shunt in 3,605 (27.2%) cases. Patients whose surgeons planned vs. planned not to shunt were more likely to have ipsilateral symptomatic stenosis (25.2% vs. 24.7%, P<.001) and severe contralateral stenosis (11.6% vs 7.5%, P<.001) and receive general anesthesia (95.7% vs 77.9%, P<.001). When surgeons planned to shunt, compared with planned not shunt, patients experienced similar 30-day stroke (.7% vs .8%, P=.49) and mortality (.6% vs .6%, P=.68) rates, but longer operative duration (116.8±49.4 vs 107.1±44.6 minutes, P<.001). On multivariable analysis, planning compared with planning not to shunt was associated with similar stroke and mortality risk, but with increased operative duration per minute (OR 1.2, 95% CI 1.14-1.18, P<.001).
Among the eCEAs, shunting was routine in 25.4%, preoperatively indicated in 1.9%, intraoperatively indicated in 4.7%, and not performed in 68%. Compared to no shunting, routine shunting and preoperatively indicated shunting were each associated with similar stroke risk, but intraoperatively indicated shunting was associated with increased stroke risk (OR 2.74, 95% CI 1.41-5.3, P.003). Increased intraoperatively indicated shunting was independently associated with previous neck radiation, non-ambulatory status, preoperative stroke-related disability, coronary artery disease, P2Y12 antagonist use, and non-white race (P<.05 for all).
CONCLUSIONS: In eCEAs, there is no difference in perioperative stroke risk when surgeons prospectively plan or plan not to shunt. When shunting is performed, shunting planned in advance is associated with lower stroke risk. 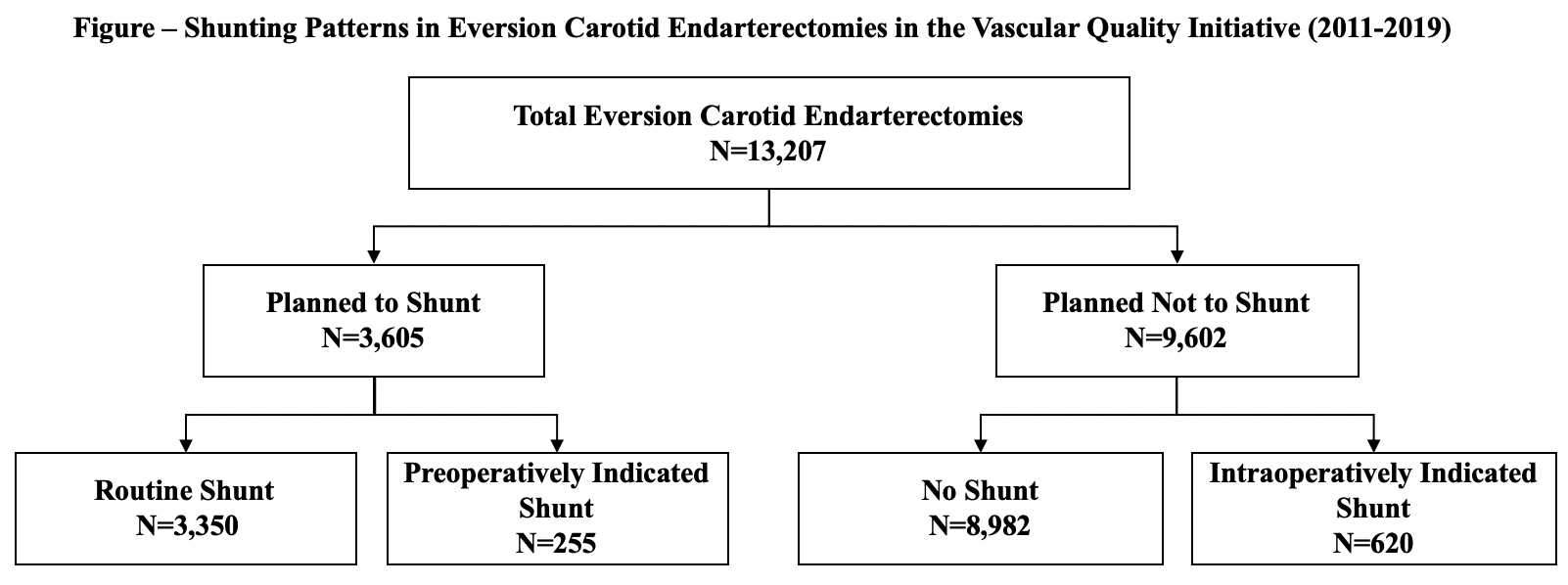
Back to 2021 ePosters
