Intravascular Ultrasound Use Is Not Associated With Differences In Operative Or Clinical Outcomes In Endovascular Repair Of Blunt Traumatic Aortic Injuries
Justin A. Smith, MD, Saideep Bose, MD, Vikram S. Kashyap, MD, Benjamin Colvard, MD.
University Hospitals Cleveland Medical Center, Cleveland, OH, USA.
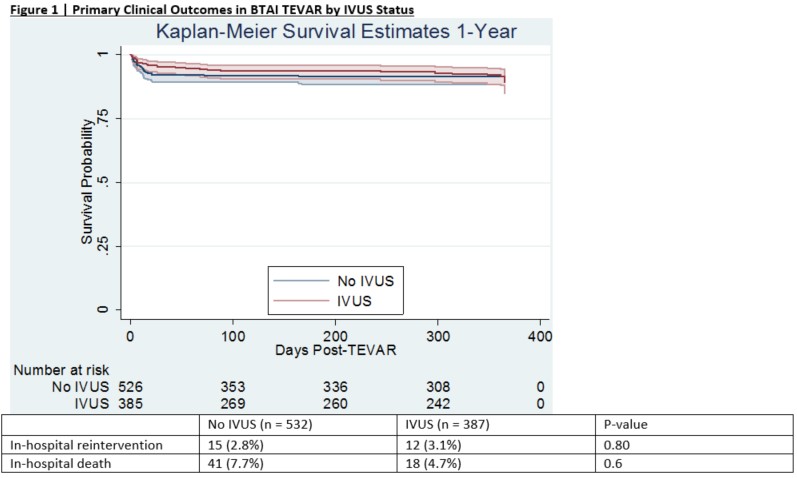
Objective: TEVAR for blunt traumatic aortic injuries (BTAI) is complicated by inaccurate aortic measurements at the time of initial CTA secondary to hypovolemic shock. IVUS use has been proposed for more accurate aortic sizing, with prior data demonstrating larger aortic sizes as measured by IVUS, potentially altering the vast majority of chosen endograft sizes. At present, no studies have examined whether IVUS affects technical or clinical outcomes. The purpose of this study was to examine the impact of IVUS on intraoperative and clinical outcomes in BTAI TEVAR. Methods: A retrospective cohort study was performed of patients undergoing TEVAR for BTAI in the VQI registry. Cohorts were defined by IVUS utilization; primary outcomes were mortality and reintervention. Results: Between 2010 and 2020, 919 patients underwent BTAI TEVAR (532 No IVUS, 387 IVUS). IVUS patients presented with higher Injury Severity Scores (36.2 vs. 42, p = 0.0004) owing to higher prevalence of chest, extremity, and external trauma. IVUS was more often used in patients with grade III injuries (49.1% vs. 56.9%, p = 0.02), and less often in ruptures (21.1% vs. 12.4%, p = 0.001). IVUS use was associated with longer fluoroscopy (7.3 vs. 8.4 minutes, p = 0.04) and procedure times (88.8 vs. 100 minutes, p = 0.01), and with a slightly higher rate of technical success (97.5% vs. 99.4%, p = 0.03). There was no observed difference in number of devices implanted or aortic zones covered by IVUS status; differences in aortic or endograft sizing could not be assessed as these data are not tracked in the VQI. IVUS use was not associated with any difference in survival or reintervention rates in-hospital or at 1-year (Figure 1); 5 reinterventions occurred across the entire patient population (4 No IVUS, 1 IVUS) in post-hospital follow-up. Conclusions: IVUS use in BTAI TEVAR is associated with a small improvement in technical success in these procedures, but is not associated with any difference in clinical outcomes. Therefore, the use of IVUS in BTAI TEVAR may represent an unnecessary adjunct, associated with longer procedure and fluoroscopy times, in patients with multiple severe traumatic injuries.
Back to 2021 ePosters
