Variability In Proximal Neck Determination Among Vascular Surgeons
Lauren Frye, DO, Michael Bounds, MD, Sam Tyagi, MD, Joseph Bobadilla, MD, Nathan Orr, MD, Eric Endean, MD, David Minion, MD.
University of Kentucky, Lexington, KY, USA.
OBJECTIVE: Proximal neck anatomy is critical to successful endovascular aneurysm repair. Although most outcomes databases rely on self-reported neck measurements, there is a wide variation in the IFU criteria of available grafts and no consensus definition of neck. The purpose of this study was to determine variability in measuring neck by vascular surgeons.
METHODS: A repository of 12 anonymized scans was created. Scans were chosen to represent a wide variety of common neck characteristics including normal, reversed conical, thrombus laden, angulated, short, suprarenal, and combinations of each. Each scan was evaluated by 7 vascular surgeons in the same practice for infrarenal neck length with no specific instructions other than to use their own personal criteria. They were also asked to provide a general description by classifying the aneurysm as either “Infrarenal,” “Juxtarenal,” “Pararenal,” “Suprarenal,” “Paravisceral,” or “Type IV TAAA.”
RESULTS: Thumbnail images along with the range of the neck length measurements submitted by the seven surgeons for each of the twelve scans are summarized in Figure 1. The pathology of the immediate infrarenal neck was severe enough for at least one of the seven surgeons to consider the aneurysm to have no infrarenal neck in 9 of the 12 cases. On the other hand, at least one of the seven surgeons considered there to be at least some infrarenal neck in all 12 cases.
The range of the neck length measurements submitted differed by as little as 2 mm (in anatomy meant to represent suprarenal pathology) to 68 mm (in a long severely angulated neck.) The standard deviation of neck length measurements for the twelve scans averaged 8 mm.
In terms of the general description, only one aneurysm was unanimously classified by all seven participants. It was the scan chosen to represent normal neck anatomy and all agreed on an “Infrarenal” description.
CONCLUSIONS: Opinions as to adequacy of infrarenal neck and how to determine neck length vary widely among vascular surgeons. Databases that rely on self-reported neck length or even anatomic classification are likely inconsistent. Methods for more simplified and standardized determinations are important for more meaningful outcomes research. 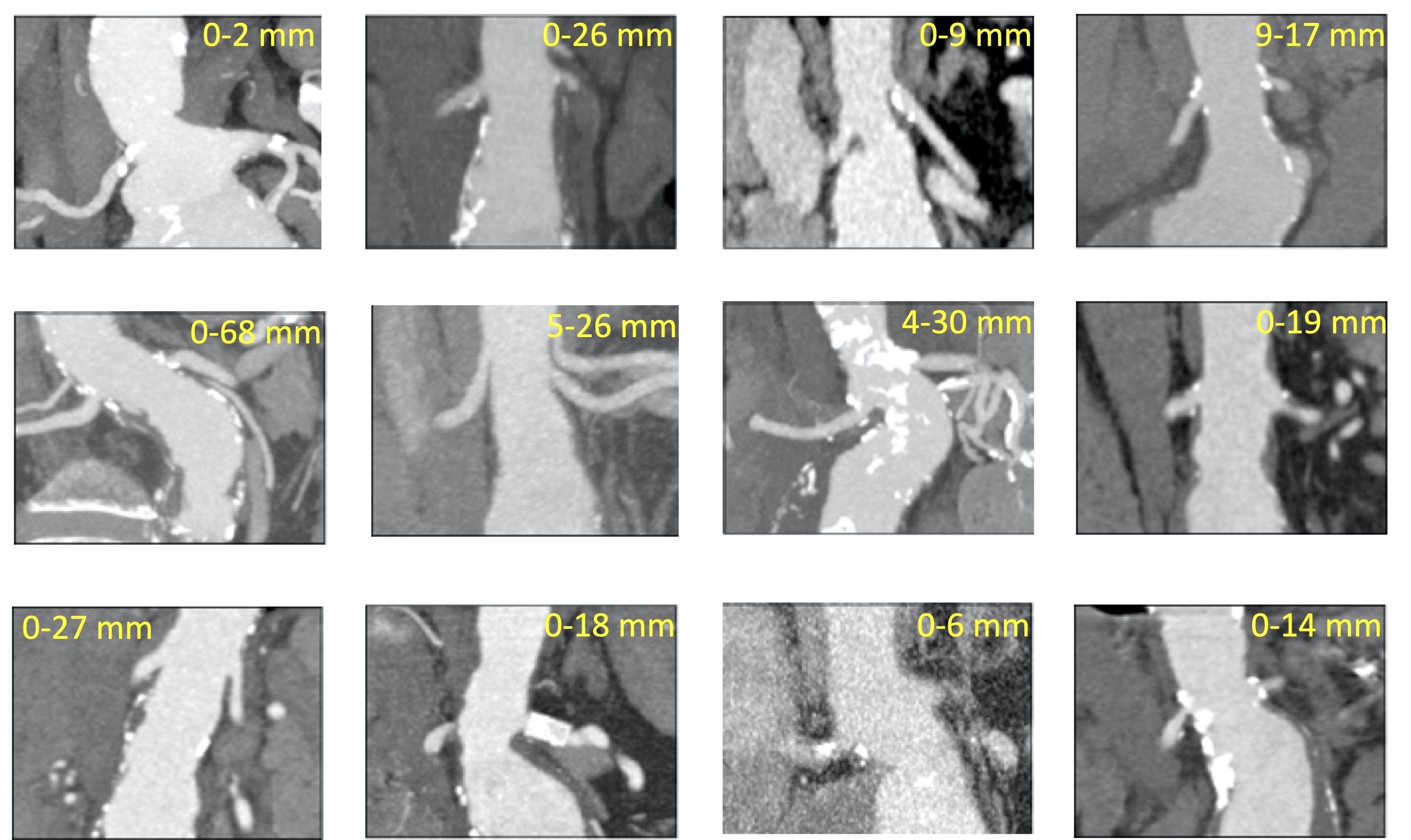
Back to 2021 ePosters
