Clinical Outcome Of Drug-Eluted Stenting (Zilver PTX) In Patients With Femoropopliteal Occlusive Disease A Single Center Experience
Ali F. AbuRahma, M.D.1, Matthew Beasley, M.D.1, Zachary AbuRahma, D.O.1, Meghan Davis, M.D.1, Elliot Adams, M.D.1, L. Scott Dean, Ph.D, MBA2, Jake Shapiro, Medical Student3, Grant Scott, M.D.1, Elaine Davis, RN, Ed.D.2.
1West Virginia University - Charleston Division, Charleston, WV, USA, 2CAMC Health Education and Research Institute, Charleston, WV, USA, 3West Virginia University School of Medicine, Charleston, WV, USA.
Background: Few industry sponsored trials reported satisfactory outcomes in the use of drug-eluting stents (DES) for treatment of femoropopliteal arterial disease. This study analyzed the early/late clinical outcome from a real world single center.
Patient populations/methods: 115 limbs treated with Zilver PTX were analyzed for: MALE (major adverse limb event: above ankle limb amputation or major intervention at 1 year), MAEs (major adverse events) (death, amputation, target lesion thrombosis/reintervention), primary patency (based on duplex ultrasound ± ABI), limb salvage and amputation free survival rates (AFS) at 1 and 2 years.
Results: Indications included claudications in 32% and critical limb ischemia (CLI) in 68%. Lesions treated included: SFA 66%, both SFA and popliteal artery (PA) 19% and PA 15%. Mean lesion length was 21 cm and 68% had total occlusion. 45% were TASC II D lesions and 55% A-C lesions. Mean follow-up was 18.4 months (1-76 months). Perioperative major morbidity rate was 8.7% with 0% mortality. MALE rate at 1 year was 17% (13.5% for claudication vs 19.2% for CLI, P=.4499). MAE rate was 30% for claudication vs 52% for CLI (P=.0392).
Overall primary patency rates at 1 and 2 years were 75% and 54% (86% and 71% for claudication vs 70% and 46% for CLI, respectively, P=.0213). Primary patency rates at 1 and 2 years were 94% and 88% for TASC A-C lesions vs 50% and 16% for TASC D lesions (P<.0001)(Figure 1). Overall freedom from MALE rate at 1 and 2 years were 85% and 79% (86% and 86% for claudication vs 84% and 74% for CLI, P=.2391). These rates were 96% and 93% for TASC A-C lesions vs 70% and 50% for D lesions, respectively (P<.0001). Limb salvage rates at 1 and 2 years were 93% and 86% (100% and 100% for claudication vs 89% and 78% for CLI, P=.012). Overall AFS rates at 1 and 2 years were 79% and 71% (93% and 82% for TASC A-C vs 59% and 59% for D lesions, P=.001).
Conclusions: Clinical outcomes after DES (Zilver PTX) in femoropopliteal arterial lesions were satisfactory for TASC A-C lesions but inferior/unsatisfactory for TASC D lesions. 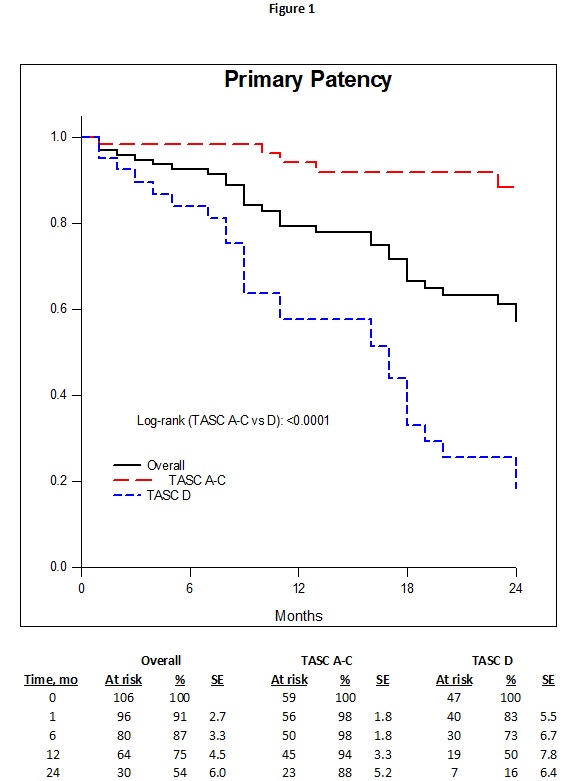
Back to 2021 ePosters
