Noninferior Limb Salvage Rates Are Attainable Without Revascularization In Patients With Chronic Limb Threatening Ischemia
Katharine L. McGinigle, MD, MPH1, Jason R. Crowner, MD1, Nikki LB Freeman, MA1, Jayer Chung, MD, MSc2, Mark A. Farber, MD1, William A. Marston, MD1.
1University of North Carolina, Chapel Hill, NC, USA, 2Baylor College of Medicine, Houston, TX, USA.
OBJECTIVES: To set therapeutic benchmarks, in 2009 the Society for Vascular Surgery published objective performance goals for chronic limb threatening ischemia (CLTI) patients. The goals are limited to 1-year outcomes for patients treated with revascularization; however, not all patients need to be revascularized to avoid limb amputation. We sought evaluate the limb salvage outcomes for patients with CLTI treated with wound care alone.
METHODS: Our cohort included patients with an incident diagnosis of CLTI (by hemodynamic and symptomatic criteria) at our institution from 2013-2017. Descriptive statistics were used to define the 2 groups - primary revascularization and primary wound care. Because treatment strategies were not randomly assigned, propensity scores accounted for differences in baseline patient characteristics. The outcomes were mortality, limb loss, amputation-free survival, and major adverse cardiac events. Differences in outcomes between the groups were defined using estimated risk differences using collaborative-targeted maximum likelihood estimation (CTMLE).
RESULTS: There were 349 incident CLTI patients; 60% male, 51% white, age 63 +/- 13 years, and 80% Rutherford 5. Most patients (79%) underwent revascularization, and 21% had wound care alone. Demographics and presenting characteristics were similar between groups. Although the revascularized patients were more likely to have femoropopliteal disease (72% vs 36%), both groups had a high rate of infrapopliteal disease (62% vs 57%). Not surprisingly, the patients in the revascularization group were less likely to have congestive heart failure (34% vs 42%), complicated diabetes (52% vs 79%), obesity (19% vs 33%), and renal failure (14% vs 28%). In the wound care group, 2-year outcomes were 65% survival, 51% amputation free survival, 19% major limb amputation, and 17% major adverse cardiac events. The wound care cohort had a 13% greater risk of death at 2 years; however, the risk of limb loss at 2 years was 12% less in the wound care cohort (Figure 1).
CONCLUSIONS:
Treatment goals and expected amputation free survival can guide revascularization, but also assure that appropriate outcomes are achieved for patients with CLTI treated without revascularizaton. Although multi-center prospective studies are needed, we demonstrate that equal, even improved, limb salvage rates are possible with wound care alone. 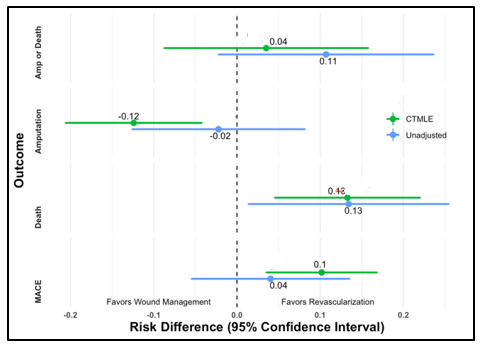
Back to 2021 ePosters
