A TALE OF TWO ARTERIES: CONTEMPORARY SUPERIOR MESENTERIC AND CELIAC ARTERY INJURY MANAGEMENT AND OUTCOMES FROM THE PROSPECTIVE VASCULAR INJURY TREATMENT REGISTRY (PROOVIT)
Joseph J. DuBose, MD1, Connor B. Kilpatrick1, Kristofer Charlton-Ouw, MD2, David V. Feliciano, MD1.
1University of Maryland, Baltimore, CA, USA, 2University of Houston, Houston, TX, USA.
OBJECTIVES: Traumatic injuries to the Superior Mesenteric Artery (SMA) and Celiac Artery (CA) are rare but challenging clinical entities. It was our intent to characterize the incidence, management and outcomes of these closely related arterial neighbors in the contemporary era.
METHODS: The American Association for the Surgery of Trauma (AAST) PROspective Observational Vascular Injury Treatment (PROOVIT) registry was used to identify the incidence of SMA and CA injuries from 2012-2109, as well as management and outcomes.
RESULTS: The PROOVIT registry captured 55 CA/SMA injuries from May 2012 through March 2019, accounting for 1.3% of all injuries enrolled (55/4358). Blunt injuries accounted for 65.5%, and median ISS was 25.5. Median age was 42, 72.7% were male. Specific injury types recorded included occlusion (7.3% [4/55]), transection (29.1% [16/55]), partial transection or flow limiting lesions (50.9% [28/55]) and pseudoaneurysm (5.5% [ 3/55]). Among patients selected for non-operative management (36.3%, 20/55), there were no failures. Open operative management was utilized for 50.9% (28/55), including initial damage control options in 40% (22/55; ligation 36.4% [20/55], temporary vascular shunt 3.6% [2/55]). Initial or post-damage control definitive open repair consisted of primary repair in 18.2% (10/55) and autologous vein interposition in the remainder 1.8% (1/55). Endovascular repair was utilized in 12.7% (7/55), in the form of stent utilization (9.1%; 5/55) and coil embolization (3.6%; 2/55). Outcomes overall, and for each injury individually are outlined in the TABLE. CA injuries were more likely to be managed with endovascular modalities (23.5% vs. 7.9%, p = 0.003). SMA injuries were more commonly repaired open (26.3% vs. 5.9%, p = 0.037) and were significantly more likely to require bowel resection due to ischemia in correlating vascular territory (18.4% vs. 0%, p = 0.039).
CONCLUSIONS: CA and SMA injuries remain challenging entities requiring the full spectrum of contemporary care options, with open repair most common for SMA and endovascular for CA treatment. SMA injuries represent a significantly greater risk for potential bowel ischemia than CA counterparts. 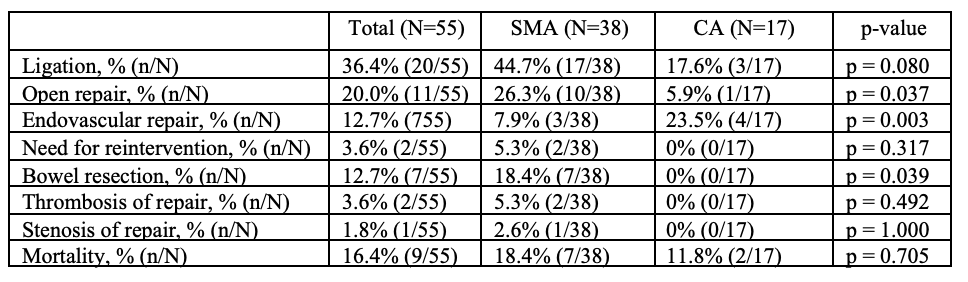
Back to 2021 ePosters
