Frailty Measurement And Implications For Cerebrovascular Disease Management In A Veteran Based Population
Sally Boyd, MD, Wayne Tse, MD, Kedar S. Lavingia, MD, Micheal F. Amendola, MD, MEHP.
Virginia Commonwealth University, Richmond, VA, USA.
OBJECTIVES: Rapid and objective preoperative assessment of patients undergoing carotid endarterectomy (CEA) remains difficult and variable. The Risk Analysis Index (RAI) is a validated medical record based assessment of frailty that has been used to predict clinical outcomes for patients undergoing surgical procedures including CEA. We applied RAI to a veteran population following CEA for asymptomatic cerebrovascular disease and examined the factors related to post-operative morbidity and mortality.
METHODS:
The Veteran Affairs Surgical Quality Improvement Program (VASQIP) data was queried for CEA procedures from 2002 to 2015 for ICD-9 and ICD-10 codes indicating asymptomatic patients. RAI was calculated based on VASQIP variable medical record extraction. Three groupings of patients were undertaken including non-frail (RAI< 30), frail (RAI 30-34) and very frail (RAI > 35).
RESULTS: Between 2002 and 2015, 41,593 asymptomatic patients underwent CEA. 40,923 (98.4%) patients were male with an average age of 68 ± 8.5 years. The cohorts contained 83.1% (n=34,554), 12.2% (n=5074), and 4.7% (n=1965) for the non-frail, frail and very frail groups respectively. Frailty was associated with increased rates of post-operative stroke, death, and any complication (p<0.05) (Table 1). Total hospital length of stay was significantly increased from non-frail (3.15 days) to frail (4.98 days) to very frail (8.79 days) (p<0.05) 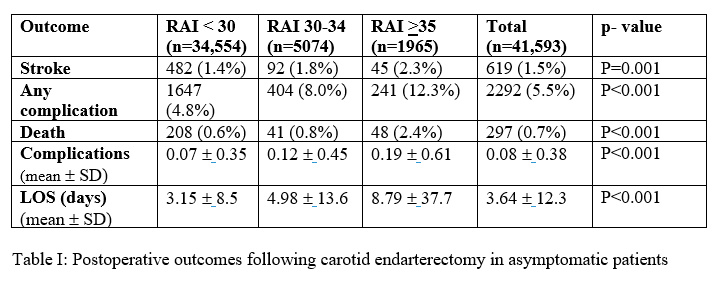 .
.
Increasing frailty predicted having one or more complications (OR 1.338, 95% CI 1.162 - 1.541 for frail and OR 1,720, 95% CI 1.385 - 2.136 for very frail, (p<0.05) and post-operative stroke in frail (OR 1.305 95% CI 1.042-1.635) and very frail (OR 1.657 1 95% CI.216-2.257) patients. Frailty was also associated with death with in very frail patients (OR 2.881, 95% CI 2.005-4.139, p<0.05) 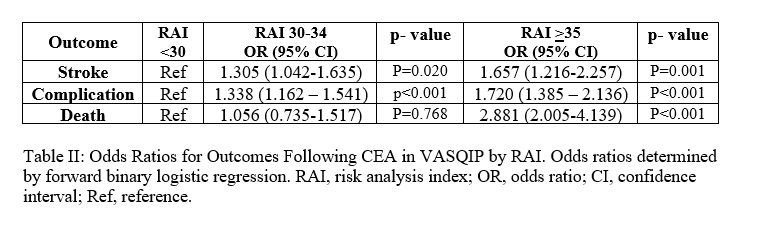 .
.
CONCLUSIONS:
Increasing frailty as determined by RAI was associated with worse post-operative outcomes in asymptomatic patients undergoing CEA. The higher RAI score cohorts were associated with higher rates of postoperative stroke, complications and death. We recommend the use of this frailty index as a screening tool to guide risk discussions with asymptomatic patients undergoing CEA.
Back to 2021 ePosters
