The Impact Of Aorto-uni-iliac Graft Configuration On The Perioperative And Short-term Outcomes Of Patients With Ruptured Abdominal Aortic Aneurysms
Rae Rokosh, MD1, Caron B. Rockman, MD1, Virendra I. Patel, MD2, Thomas Maldonado, MD1, Neal S. Cayne, MD1, Glenn R. Jacobowitz, MD1, Karan Garg, MD1.
1NYU Langone Health, New York, NY, USA, 2Columbia University Medical Center, New York, NY, USA.
Objectives: Endovascular aneurysm repair (EVAR) has improved outcomes for ruptured abdominal aortic aneurysms (rAAA) compared to open repair. We examined the impact of aorto-uni-iliac (AUI) versus standard bifurcated endograft configuration on outcomes in rAAA.
Methods:Patients 18 or older in the VQI database who underwent EVAR for rAAA from 1/2011- 4/2020 were included. Patient characteristics were analyzed by graft configuration: AUI or standard bifurcated. Rationale for chosen configuration, such as suitable aortoiliac anatomy, is not captured in the VQI. Primary and secondary outcomes included 30-day mortality, post-operative major adverse events (MAE; myocardial infarction, stroke, heart failure, mesenteric ischemia, lower extremity embolization, dialysis requirement, re-operation, pneumonia or re-intubation) and 1-year mortality.
Results: 2717 patients were included: 151 had AUI and 2566 had standard bifurcated repair. There was no significant difference between groups in terms of age, major medical comorbidities, anatomic aortic neck characteristics, or rates of conversion to open repair. Patients undergoing AUI were more likely female (30.5% vs. 21.6%, p=0.011) and had a history of CHF (18.8% vs. 11.9%, p=0.013). Perioperatively, patients undergoing AUI had a significantly higher incidence of cardiac arrest (14.6% vs. 7%, p<0.001), increased intra-operative blood loss (1.3L vs. 0.6L, p<0.001), longer operative duration (218min vs. 138min, p<0.0001), higher incidence of MAE (46.3% vs. 33.3%, p=0.001), as well as prolonged ICU (7 vs. 4.7days p=0.0006) and overall hospital length of stays (11.4 vs. 8.1days, p=0.0003). Kaplan-Meier survival analyses demonstrated significant differences in 30-day (31.1% vs. 20.2%, log-rank p=0.0013; Figure 1) and 1-year mortality (41.7% vs. 27.7%, log-rank p=0.0001). By Cox regression analysis, perioperative cardiac arrest (HR 5.8, CI 4.7-7.1, p<0.001) and significant intraoperative blood loss (HR 2.8, CI 2.4-3.5, p<0.001) but not graft configuration (HR 0.9, CI 0.7-1.3, p=0.724) were the strongest independent associations with all-cause 30-day mortality.
Conclusions: The use of AUI configuration for rAAA appears to be associated with worse perioperative and 1-year outcomes compared to a bifurcated graft configuration. Although graft configuration was not an independent predictor of increased mortality on multivariate analysis, standard bifurcated graft configuration may be the preferred approach in the management of rAAA unless AUI configuration is mandated by patient anatomy. 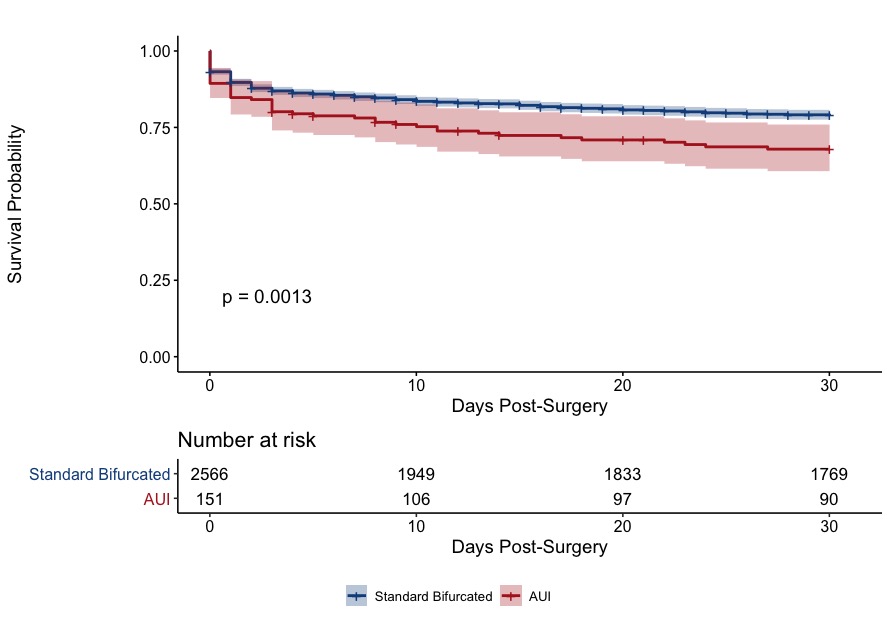
Back to 2021 ePosters
