Human Immunodeficiency Virus Infection Is Associated With Advanced Presentation And In-hospital Mortality After Surgery In Patients With Peripheral Arterial Disease
Lillian M. Tran, M.D., Guangzhi Cong, M.D. Ph.D., Mohammad H. Eslami, M.D. M.P.H, Ulka Sachdev, M.D..
University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
OBJECTIVE
Several studies have demonstrated an increased risk of developing peripheral arterial disease (PAD) in patients living with human immunodeficiency virus (HIV). However, the effect of concurrent HIV infection on PAD severity and treatment outcomes has not been established. This study assesses inpatient outcomes of PAD interventions in patients with and without HIV infection.
METHODS
The National Inpatient Sample (2003-2017) was used to identify patients undergoing lower extremity revascularization or amputation for PAD using ICD-9 and ICD-10 diagnosis and -CM procedure codes. Patients from this cohort diagnosed with HIV infection were compared to those without an HIV diagnosis. Nearest neighbor 1:1 matching was performed to create matched cohorts. Adjusted statistical analyses on demographics, clinical characteristics and perioperative inpatient outcomes were performed following matching.
RESULTS
A total of 224,912 patients between ages 18-85 years were admitted with PAD and underwent a lower extremity procedure. 1,264 (0.56%) of these patients were also diagnosed with HIV infection. Patients with morbid acquired immune deficiency syndrome (AIDS)-related complications were excluded from the study. The HIV-positive group was more likely to be black (32.8% vs 40.3%, p<0.001), and more likely to have Medicaid for primary insurance coverage (13.6% vs. 7.4%, p<0.001). HIV+ patients were more likely to present with critical limb ischemia (CLI;57.3% vs 43.1%, p<0.001) and undergo major amputations (28.6% vs 9.8%, p<0.001). In-hospital mortality (4.0% vs 1.8%, p=0.001) and length of hospital stay (7.8 ± 7.3 vs 6.5 ± 76.3, p<0.001) were significantly higher in the HIV-positive group. Adjusted multivariate logistic regression analysis also demonstrated HIV infection to be a significant, independent predictor of inpatient mortality (OR 2.46 [1.37-4.40], p=0.003).
CONCLUSIONS
PAD patients with HIV are more likely to present with limb threatening ischemia, and suffer from limb loss and death when compared to a matched HIV-negative cohort. Even when adjusting for race and socioeconomic factors, HIV infection predicted mortality following intervention for PAD. These findings suggest that chronic HIV infection may exacerbate morbidity associated with vascular disease. 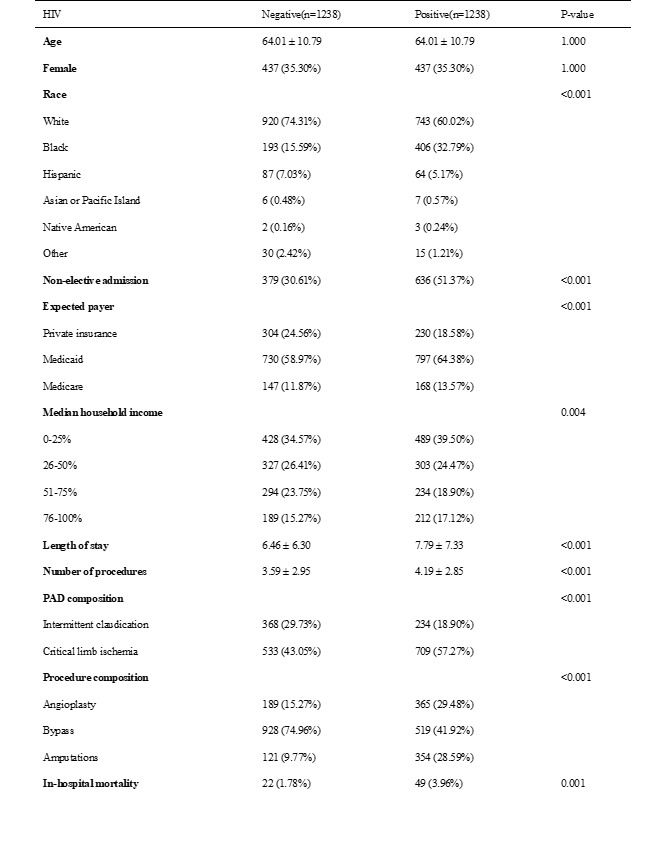
Back to 2021 ePosters
