Outcomes Of Femoropopliteal Bypass And Endovascular Interventions For Tasc C And D Lesions Among Patient With Premature Peripheral Artery Disease
Tanner Kim, MD1, Yawei Zhang, MD, PhD, MPH2, Jonathan Cardella, MD1, Raul Guzman, MD1, Cassius Iyad Ochoa Chaar, MD, MS1.
1Yale University School of Medicine, New Haven, CT, USA, 2Yale University School of Public Health, New Haven, CT, USA.
OBJECTIVES: Patients with premature peripheral artery disease (PAD), defined by age ≤ 50 at presentation, have poor outcomes with open and endovascular lower extremity revascularization (LER). It is unclear if either strategy is associated with better outcomes as comparative studies are limited to case series in this patient population. The aim of this study is to compare outcomes of patients with premature PAD undergoing bypass or endovascular revascularization for advanced femoropopliteal disease.
METHODS: All patients with premature PAD undergoing isolated femoropopliteal LER in the Vascular Quality Initiative infrainguinal bypass and peripheral vascular intervention files were reviewed from 2003 through 2019. Propensity score matching (1:1) was performed between patients undergoing femoropopliteal bypass and endovascular interventions for isolated femoropopliteal Trans-Atlantic Classification System (TASC) C or D lesions. One-year outcomes including reintervention, patency, major amputation, and mortality were analyzed.
RESULTS: There were 902 patients who underwent isolated femoropopliteal endovascular intervention, and 1,636 patients who underwent femoropopliteal bypass. Patients undergoing endovascular intervention were more likely to have diabetes (68.85% vs 53.97%, P<.001), coronary artery disease (31.04% vs 22.98%, P<.001), renal failure requiring dialysis (14.19% vs 7.15%, P<.001), and claudication (45.05% vs 36.61%, P<.001) compared with those undergoing bypass. After propensity matching, there were 466 patients in each group with no significant differences in baseline characteristics. Perioperative morbidity was higher with femoropopliteal bypass compared with endovascular intervention (12.02% vs 7.94%, P=.038), but major amputation and mortality were no different. At one-year, patients undergoing femoropopliteal bypass were less likely to require reintervention (16.95% vs 25.15%, P=.012). However, there was no difference in major amputation (7.72% vs 7.91%, P=.928) or mortality (5.15% vs 5.15% P=1.00). Propensity matching was also performed between premature PAD patients who underwent femoropopliteal bypass with great saphenous vein and isolated femoropopliteal endovascular interventions, and the outcomes were similar.
CONCLUSIONS: Among patients with premature PAD, major amputation and mortality did not differ between bypass and endovascular interventions for isolated femoropopliteal disease at one-year. However, reinterventions were significantly higher with endovascular intervention. 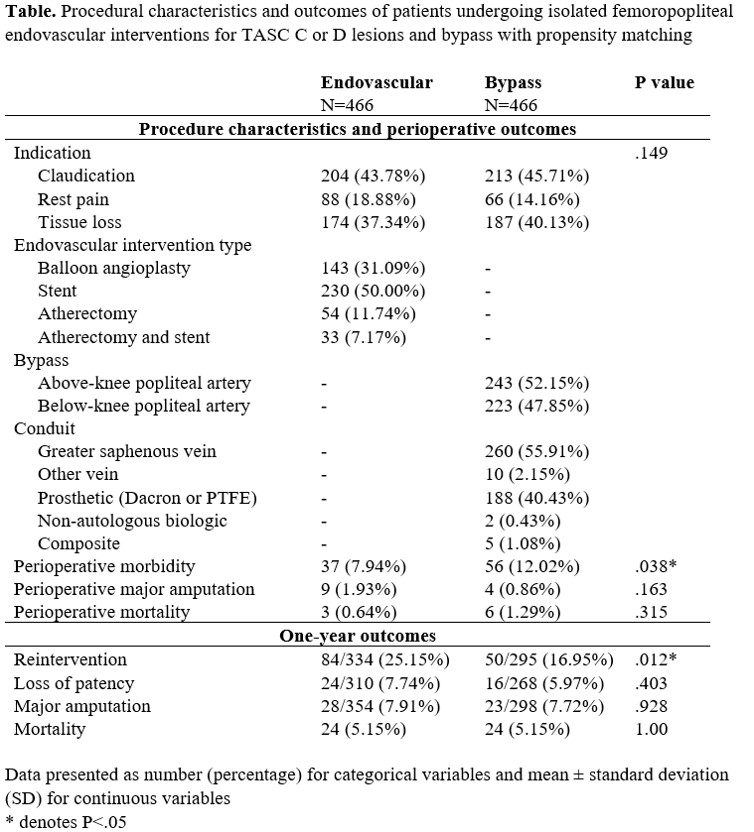
Back to 2021 ePosters
