Feasibility And Utility Of Intracranial Imaging During Tcar
Christopher M. Faries, Justin M. George, MD, Kelsey Berger, MD, Peter V. Cooke, BA, Rami O. Tadros, MD, Peter L. Faries, MD.
Icahn School of Medicine at Mount Sinai, New York, NY, USA.
OBJECTIVES: Transcarotid artery revascularization(TCAR) is a validated option for carotid intervention in high risk patients. In the pivotal ROADSTER trial, there was a finite (1.4%) incidence of intraprocedural cerebrovascular accident(CVA). TCAR is often performed using general anesthesia which limits the capacity to assess neurological function intraoperatively. When performing transfemoral carotid artery stenting, intracranial imaging is performed before and after intervention in order to identify intraprocedural complications; however, the current Instructions for Use for TCAR do not include intracranial imaging. The objective of this study is to demonstrate feasibility and utility of cerebral angiography during TCAR.
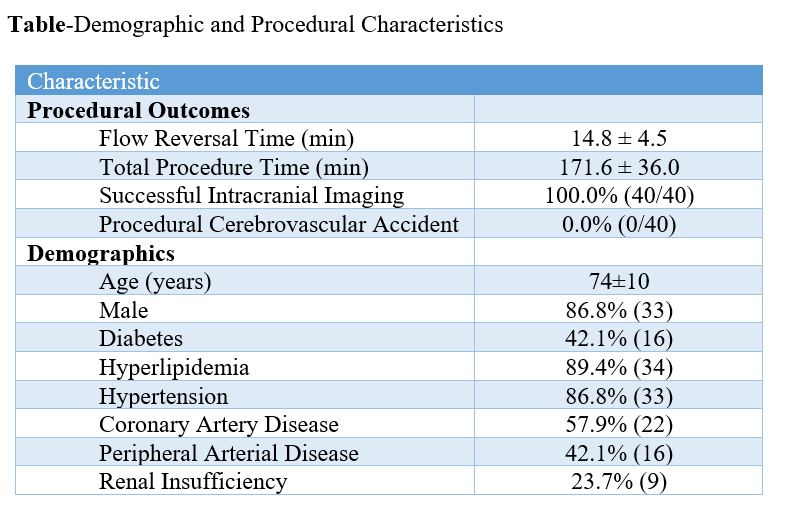
METHODS: A single center pilot program was created to prospectively assess the feasibility of intracranial angiographic imaging during TCAR. Preoperative demographic data and procedural characteristics were collected and analyzed. Lateral and Towne’s views were obtained in all patients prior to and following TCAR with flow reversal. Primary end point was technical success of the imaging procedure. Secondary endpoints were TCAR procedural success, duration of flow reversal, and CVA. RESULTS: 40 consecutive patients were enrolled in the feasibility trial. Mean age was 74±10 years, 86.8% were male, 42.1% had diabetes, 89.4% hyperlipidemia, 86.8% hypertension, and 57.9% coronary artery disease. Mean flow reversal time was 14.8±4.5 minutes and mean procedure time 171.6±36.0 minutes. Mean follow up was 2.5±2.1 years. There was a 100% success rate in performing intracranial imaging with 0% CVA.(Table) This allowed real time characterization of intracranial perfusion and the potential for identification of possible CVA. The benefits of intraprocedural diagnosis of CVA include rapid intervention and neurological rescue, avoiding reopening of carotid cutdown site, avoidance of femoral access should neurological rescue procedures be required, and ability to administer lytic agents as the surgical incision is still open and hemostatic control can be achieved. There is no significant disadvantage to intracranial imaging as flow reversal times in our study are comparable to the 12.9±8.6 minutes published in the ROADSTER trial without intracranial imaging.
CONCLUSIONS: Intracranial imaging prior to and after initiation of flow reversal is feasible in TCAR. This technique allows intraprocedural identification of CVA and provides the potential for rapid and appropriate treatment.
Back to 2022 Abstracts
