Expanding Our Capacity To Train Vascular Surgeons: Results Of A National Initiative
Malachi G. Sheahan, MD1, Shivik Patel, MD1, Kapland Owens, MD1, Claudie Sheahan, MD1, Jean Bismuth, MD2, William D. Jordan, Jr., MD3, Michel Makaroun, MD4, Jeffrey Jim, MD5.
1Louisiana State University Health Sciences Center, New Orleans, LA, USA, 2Methodist Hospital, Houston, TX, USA, 3Emory University School of Medicine, Atlanta, GA, USA, 4University of Pittsburgh School of Medicine, Pittsburgh, PA, USA, 5Allina Health, Minneapolis, MN, USA.
OBJECTIVES: In 2018, the Society for Vascular Surgery and the Association for Program Directors in Vascular Surgery formed a task force to address the critical workforce shortage facing our specialty. A key aim was to assess and mitigate the barriers to creating new vascular training programs.
METHODS: A list of potential new vascular surgery training programs was developed by identifying general surgery residencies without associated vascular programs as well as large private vascular practices without fellowships. Each potential site was then contacted by a member of the task force. Additional program development mentorship was provided by task force members.
RESULTS: Of the 311 ACGME accredited general surgery programs, 172 (55%) did not have an associated vascular residency or fellowship. Of these, 90 were identified as redundant or a poor fit due to a lack of vascular faculty. Vascular surgery faculty in the remaining 82 programs were interviewed by our task force members. When asked to identify their main barrier to program development, the most commonly cited was confusion regarding the application process (43%, 35/82) followed by a lack of faculty (27%, 22/82), and insufficient financial support (21%, 17/82). Additionally, 12 large private practices were identified and contacted as potential sites for vascular fellowships. Of these only two (17%) expressed an interest in starting a program within the next three years. The most common barriers cited were financial (50%, 6/12), administrative (42%, 5/12), and lack of interest (42%, 5/12). In the three years prior to the task force formation a total of seven new vascular programs were approved by the ACGME. In the two years the task force was active, 20 new programs were approved (Figure 1).
CONCLUSIONS: While a lack of vascular faculty and financial restrictions remain significant barriers to the formation of new vascular training programs, confusion over the initial application process has become a principal issue. A coordinated national mentorship program may alleviate this barrier. 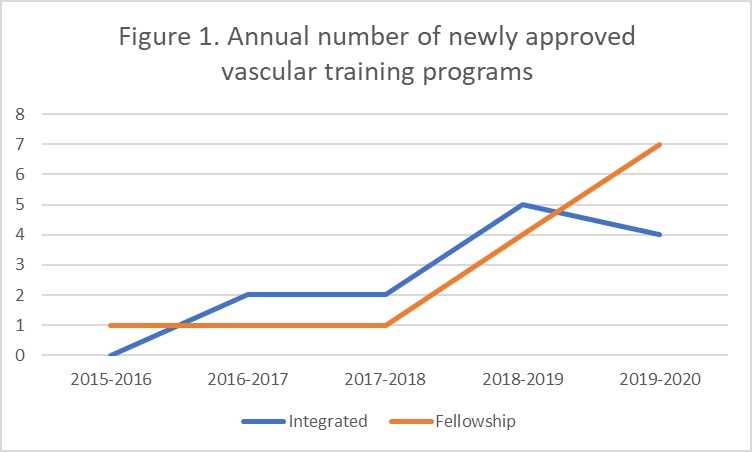
Back to 2022 Abstracts
