Disease Burden Is Greater In Patients With Deep Venous Reflux, But Treatment Of Associated Superficial Venous Reflux Remains Safe And Effective
Chong Li, MD1, Caron Rockman, MD1, Glenn R. Jacobowitz, MD1, Thomas S. Maldonado, MD1, Lowell S. Kabnick, MD2, Neal Cayne, MD1, Todd L. Berland, MD1, Mikel Sadek, MD1.
1New York University, New York, NY, USA, 2United Vein Centers, Tampa, FL, USA.
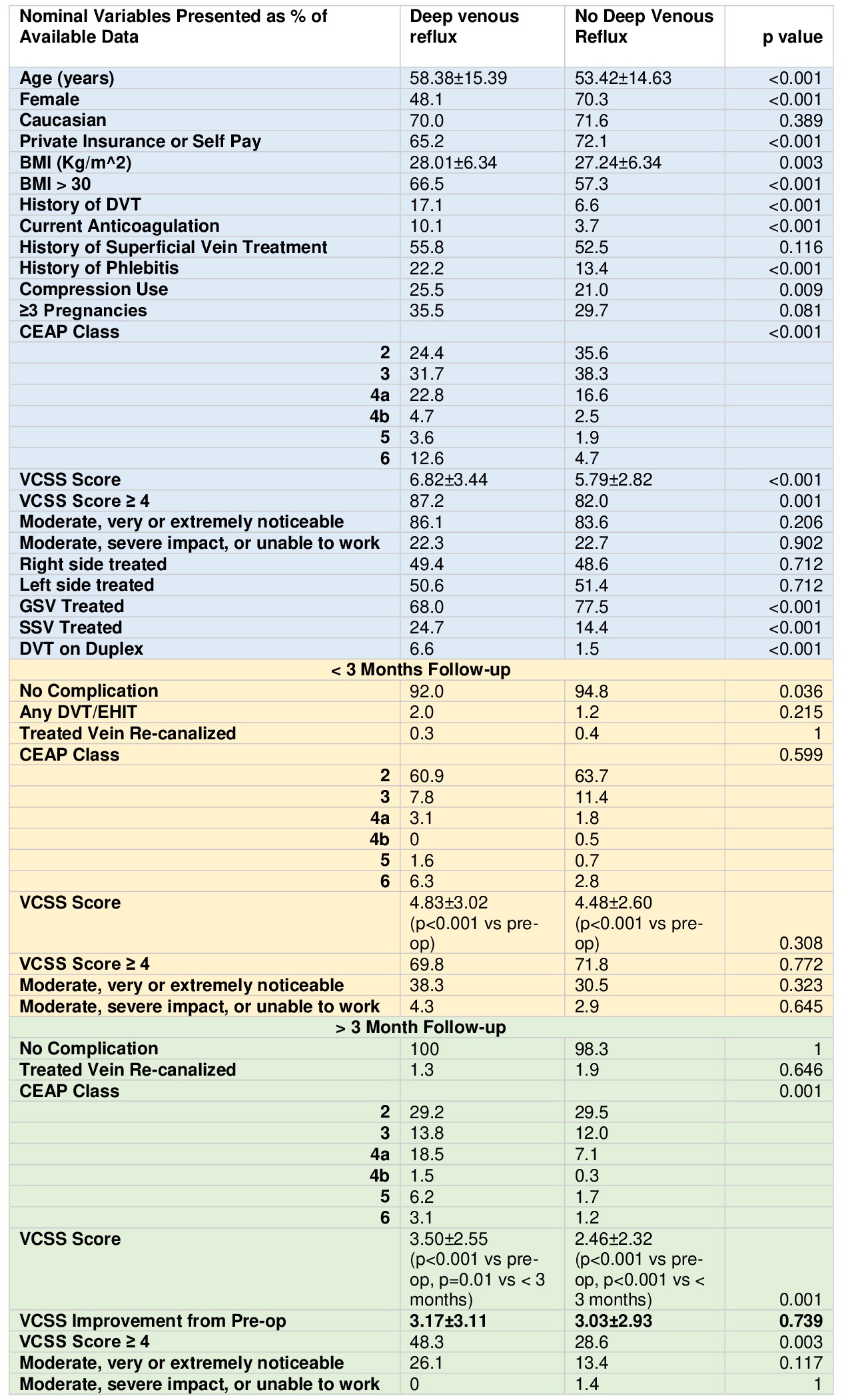
Objective The incidence of deep venous reflux (DVR) in a real-world practice of patients undergoing treatment for chronic venous insufficiency remains underreported. Moreover, the safety and efficacy, as well as clinical outcomes in patients with DVR undergoing superficial venous treatments have not been investigated. This study sought to address these questions. Methods This study was a retrospective review of the institutional vascular quality initiative database between June 2016 to June 2021. Consecutive patient-limbs were identified who underwent superficial venous intervention and had duplex evaluation of the corresponding limb. The cohort was divided into those with and without DVR. The incidence of DVR was determined, and the primary outcome was venous clinical severity score (VCSS) score on > 3 months follow-up. Secondary outcomes included incidence of post-procedural DVT/EHIT, CEAP, and impact on work. Both univariate and multivariate logistic regression analyses were performed. Results A total of 8,456 patient-limbs were evaluated (DVR: 644 and NO DVR: 7812) for an incidence of 7.6%. DVR was associated with older age, higher BMI, SVT history, DVT history, anticoagulation, compression use, and higher CEAP and VCSS scores. The majority of patients underwent endothermal ablation of the GSV or SSV. On univariate analysis, both groups improved significantly in VCSS score at <3 months follow-up (4.83±3.02 vs 4.48±2.60, P=0.308). The VCSS score again improved significantly at >3months follow-up, but was significantly higher in the DVR cohort (3.50±2.55 vs 2.46±2.32, P<0.001). When evaluating the differences in VCSS over time, both cohorts improved an equal amount (3.17±3.11 vs 3.03±2.93, P=0.739). On multivariate logistic regression, deep venous reflux was not associated with an increased VCSS on follow-up but was associated with decreased postoperative DVT/EHIT (OR 0.1, 0.02-0.51, P=0.005). Appearance and impact on work did not differ between the two groups on follow-up. Conclusions Although DVR is associated with a higher burden of chronic venous insufficiency and DVT, treatment of the superficial veins in these patients is at least as safe and effective, with clinical and patient-reported outcomes equal to those without DVR. Additional evaluation may help to confirm if DVR is protective against the development of a thrombotic complication.
Back to 2022 Abstracts
