Impact Of Frailty On Patients Undergoing Percutaneous Peripheral Vascular Intervention
Abdul Kader Natour, MD, Alexander Shepard, MD, Mitchell Weaver, MD, Timothy Nypaver, MD, Loay Kabbani, MD.
Henry Ford Health System, Detroit, MI, USA.
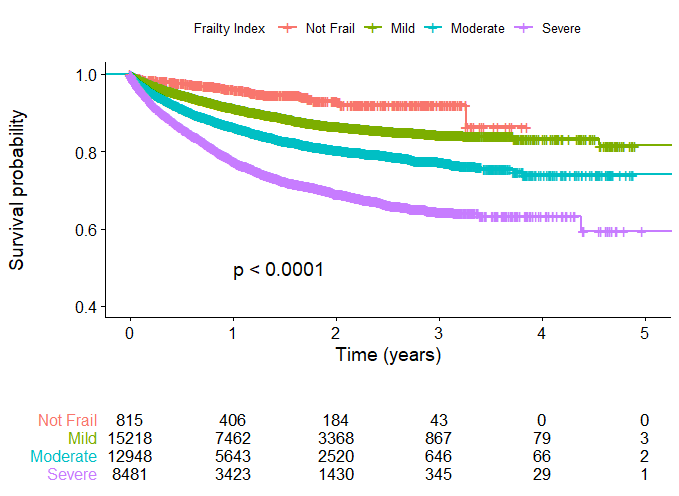
Objective: The Vascular Quality Initiative (VQI)® database was used to determine whether the 5-factor modified frailty index score (mFI-5) was associated with post-operative outcomes in critical limb threatening ischemia (CLTI) patients undergoing percutaneous peripheral vascular interventions (PVIs). Methods: The national VQI dataset was queried for all PVIs performed between 2010 and 2019 in CLTI patients. Using the mFI-5, each patient was assigned a numeric score ranging from 0-5 depending on the presence (score of 1) or absence (score of 0) of the following comorbidities: diabetes, hypertension, congestive heart failure, chronic obstructive pulmonary disease, and functional status limiting independence. Patients were then categorized as no frailty (0), mildly (1-2), moderately (3), or severely frail (4-5). Multivariate models were used to evaluate the association between frailty and 30-day mortality, length of stay (LOS), in-hospital major adverse limb events (MALE), and 1-year/overall survival. Kaplan-Meier curves were used to compare the survival time based on frailty severity. Results: There were 37,484 patients with CLTI who underwent PVI. Mean age was 70 years (±12), 58% were male, and 73% were white. Forty percent of the patients were mildly frail (N=15,226), 35% were moderately frail (N=12,956), and 23% were severely frail (N=8,487). Baseline characteristics (Age, Female, and African American) and comorbidities (BMI, CAD, Dialysis, and Smoking) were associated with increased frailty. When compared to non-frail patients, severely frail patients were more likely to present with advanced CLTI (79% vs 45%, P<0.001) and experience higher MALE (24% vs 10%, P<0.001). On univariate analysis, 30-day mortality, MALE, LOS, and 1-year/overall survival was significantly associated with the level of frailty. These associations persisted on multivariate models. Kaplan-Meier survival was associated with the level of frailty (P<0.001) (Figure 1). Conclusions: In this cohort, frail patients tend to present with more advanced CLTI. CLTI Patients undergoing PVIs with higher mFI-5 scores are at independent increased risk of 30-day death, in-hospital MALE, LOS, and decreased 1-year/overall survival. The mFI-5 is a simple and excellent predictor of outcome in CLTI patients undergoing PVIs. The presence and degree of frailty should be important components of preoperative risk stratification for CLTI patients undergoing PVIs.
Back to 2022 Karmody Posters
