Discharge On A Direct Oral Anticoagulant Does Not Improve Reintervention Rates In Peripheral Endovascular Procedures
Elizabeth A. Andraska, MD, MS1, Adham Abou Ali, MD1, Mohammad H. Eslami, MD, MPH1, Abhisekh Mohapatra, MD, MSc2, Michael Madigan, MD1.
1University of Pittsburgh Medical Centers, Pittsburgh, PA, USA, 2Massachusetts General Hospital, Boston, MA, USA.
Objectives: Recent randomized trials suggest that treatment with low dose direct oral anticoagulation (DOAC) after infraingunal bypass improves limb related outcomes. The objective of this study was to examine the effect of DOAC use in patients undergoing infrainguinal endovascular intervention.
Methods: This study utilized the Vascular Quality Initiative (VQI) Peripheral Vascular Intervention database from 2009-2020. Patients undergoing first time, elective infrainguinal endovascular intervention with at least one follow-up visit were included in the analysis. Patients on pre-operative anticoagulation were excluded. Patients discharged on a DOAC were compared to those discharged on no anticoagulation. One year freedom from reintervention was the primary outcome. Freedom from reintervention was plotted with Kaplan-Meier curves and compared using log rank testing. Propensity scores of patients in the DOAC and no anticoagulation groups were calculated by age, gender, smoking status, degree of pre-operative symptoms, and TASC score. Proportional hazard Cox regression was performed with propensity scores to evaluate risk factors for reintervention.
Results: 48,892 patients from the VQI were included in the analysis. Propensity matching led to549 patients in the DOAC group and 38,662 patients in the no anticoagulation group. 72.6% of patients in the DOAC group had either rest pain or tissue loss compared to only 51.1% of the patients in the no anticoagulation group (p<0.01). One-year freedom from reintervention was 89.9% for the DOAC group and 92.5% for the no anticoagulation group (log rank <0.01, Figure 1). Adjusted propensity score analysis confirmed this finding (p = 0.03). 71.4% of reinterventions for patients on DOAC were endovascular while 77.0% of reinterventions for patients on no anticoagulation were endovascular (p = NS). Bleeding complications were no different between groups (2.1% DOAC vs. 1.9% no anticoagulation). The adjusted comparison using propensity matching identified discharge with a DOAC as a risk factor for reintervention at one year (Hazard ratio, 1.4; 95% confidence interval, 1.2-1.6; P = 0.03).
Conclusions: DOAC does not result in improved outcomes for patients undergoing peripheral endovascular interventions. Randomized trials are necessary to evaluate the safety and efficacy of DOAC in peripheral endovascular interventions. 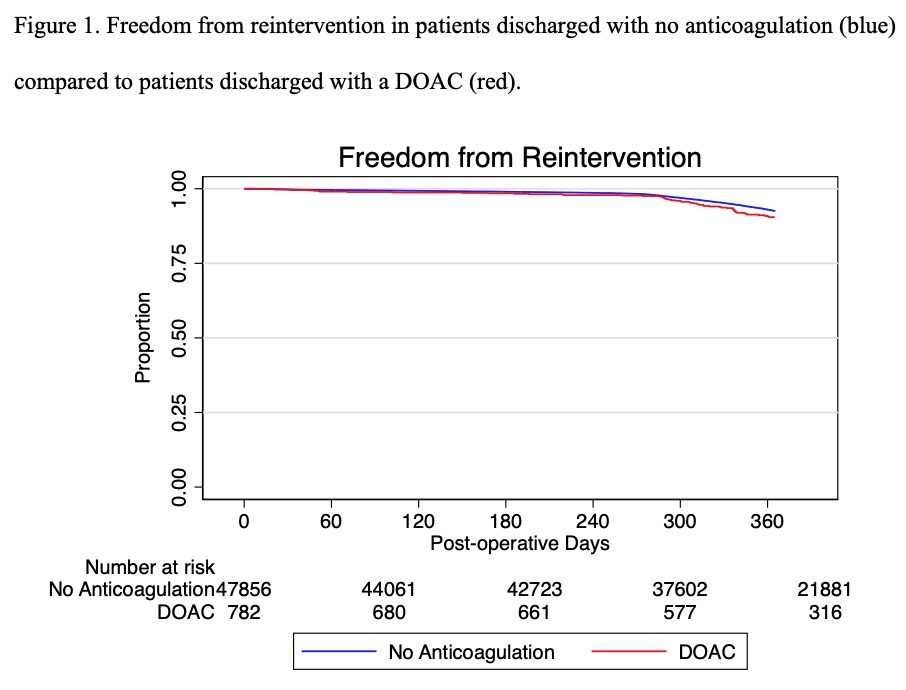
Back to 2022 Karmody Posters
