Aortic Size Index Accounts For Sex-Specific Differences In Abdominal Aortic Aneurysm Diameter At The Time Of Rupture.
Jake F. Hemingway, MD, Myra Ahmad, BS, Blake E. Murphy, MD, Elina Quiroga, MD, Nam Tran, MD, Niten Singh, MD, Benjamin W. Starnes, MD, Sara L. Zettervall, MD MPH.
University of Washington, Seattle, WA, USA.
OBJECTIVES: Prior studies examining sex-related differences in outcomes following abdominal aortic aneurysm (AAA) repair suggest worse outcomes among women due to lower rates of endovascular repair (EVAR), anatomic differences, and higher rates of rupture despite smaller AAA diameters. The aortic size index (ASI) has been proposed as a surrogate marker of rupture risk in women to account for these sex-specific differences. However, no studies have compared anatomic variations and outcomes between men and women following ruptured AAA (rAAA).
METHODS: A retrospective review of all rAAA patients treated at a single academic center between January 2002 and December 2018 was performed. The Dubois and Dubois formula was used to calculate ASI. Demographics and outcomes between men and women were compared using the Student t-test and Chi-Squared test. The distributions of aneurysm diameter and ASI were compared using the Kolmogorov-Smirnov test. Predictors of post-operative morbidity and mortality were assessed with multivariable analysis.
RESULTS: 239 patients met inclusion criteria. Women (n=45, 19%) had higher rates of chronic obstructive pulmonary disease (43% vs. 23%, p=.010) and smaller AAA diameters (Figure 1A, p=.03). ASI was comparable (Figure 1B). Although a similar percentage of women had anatomy suitable for EVAR (53% vs. 66%), women were less likely to undergo EVAR (36% vs. 56%, p=.02). There were no differences in outcomes including 30-day mortality (27% vs. 28%), post-operative respiratory failure (38% vs. 35%), renal failure (13% vs. 20%), or major adverse cardiac events (7% vs. 10%). Neither ASI (p=.72), nor AAA diameter (p=.77), were predictive of 30-day mortality on multivariable analysis. The differences seen in AAA diameter based on gender (Figure 1A) disappeared when ASI was calculated (Figure 1B, p=.46). CONCLUSIONS: Despite lower rates of EVAR, following repair of ruptured AAA, men and women achieve similar perioperative outcomes, and the ASI accounts for sex-specific differences seen in AAA diameter. An aggressive approach to management should be applied to all patients treated with ruptured AAA regardless of sex. 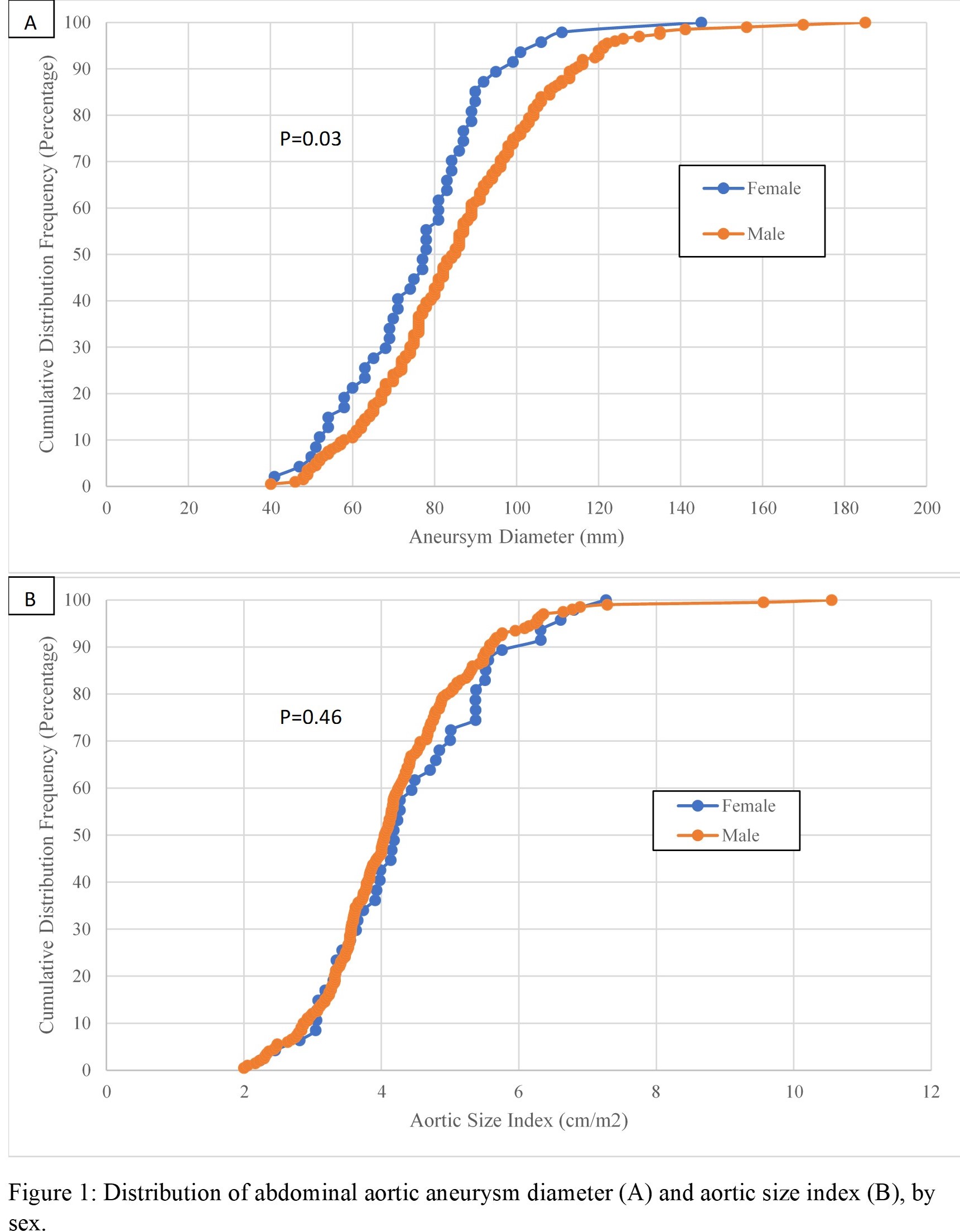
Back to 2022 Abstracts
