Transcarotid Artery Revascularization Associated With Reduced Adverse In-hospital Events And Better Long-term Survival Compared To Transfemoral Carotid Artery Stenting
Jerry Zhu, Ajit Rao, MD, Windsor Ting, MD, Daniel Han, MD, Rami Tadros, MD, David Finlay, MD, Ageliki Vouyouka, MD, Michael Marin, MD, Peter Faries, MD.
The Mount Sinai Hospital, New York, NY, USA.
OBJECTIVES: Research is limited on the impact of symptomatic status on adverse events following transcarotid artery revascularization (TCAR). We compared the association of symptomatic status with in-hospital outcomes and long-term survival after TCAR to transfemoral carotid artery stenting (TFCAS). METHODS: Data from patients in the Vascular Quality Initiative database undergoing TCAR (Jan 2017 to Apr 2020) or TFCAS (May 2005 to Apr 2020) was analyzed. Symptomatic status was defined as transient ischemic attack (TIA) and/or stroke within 180 days prior to procedure. Adverse in-hospital outcomes were analyzed with Chi-Square and 3-year survival was estimated using Kaplan-Meier. Multivariate logistic regression and Cox regression were used to adjust for significant between-group differences in baseline characteristics. RESULTS: 7,158 patients underwent TCAR (symptomatic:2,574, asymptomatic:4,584) and 18,023 patients underwent TFCAS (symptomatic:6,195, asymptomatic:11,828) during the study period. TCAR patients were generally older, white, smokers, and had more comorbidities than TFCAS. Among both asymptomatic and symptomatic patients, TCAR was associated with a significant decrease in the odds of in-hospital stroke (asymptomatic OR:0.54, 95%CI:0.38-0.77, P<.001; symptomatic OR:0.63, 95%CI:0.46-0.87, P=0.004) and TIA/stroke (asymptomatic OR:0.56, 95%CI:0.42-0.76, P<.001; symptomatic OR:0.63, 95%CI:0.48-0.82, P<.001) compared with TFCAS. TCAR was also associated with decreased odds of death (OR:0.40, 95%CI:0.21-0.76, P=0.005), stroke/death (OR:0.47, 95%CI:0.34-0.65, P<.001), and stroke/death/MI (OR:0.53, 95%CI:0.40-0.71, P<.001) among asymptomatic patients. An even greater decrease in the odds of death (OR:0.18, 95%CI:0.10-0.30, P<.001), stroke/death (OR:0.41, 95%CI:0.31-0.54, P<.001), and stroke/death/MI (OR:0.45, 95%CI:0.35-0.58, P<.001) was observed among symptomatic patients. Specifically, TFCAS was associated with increased rate of in-hospital death among symptomatic patients (2.7%) compared to asymptomatic patients (0.6%), which reduced the odds ratio of in-hospital death in TCAR versus TFCAS. In the adjusted three-year survival of symptomatic patients, TCAR was associated with a 42% reduction in hazard (HR:0.58, 95%CI:0.48-0.71, P<.001) compared to TFCAS (Figure 1A). Asymptomatic patients also benefited, as TCAR was associated with a 36% reduction in hazard (HR:0.64, 95%CI:0.53-0.78, P<.001) compared to TFCAS (Figure 1B). CONCLUSIONS: These results indicate that TCAR resulted in reduced adverse in-hospital outcomes compared to TFCAS among asymptomatic and symptomatic patients. TCAR had a short-term survival benefit notable among symptomatic patients and long-term survival benefit sustained three years after surgery. 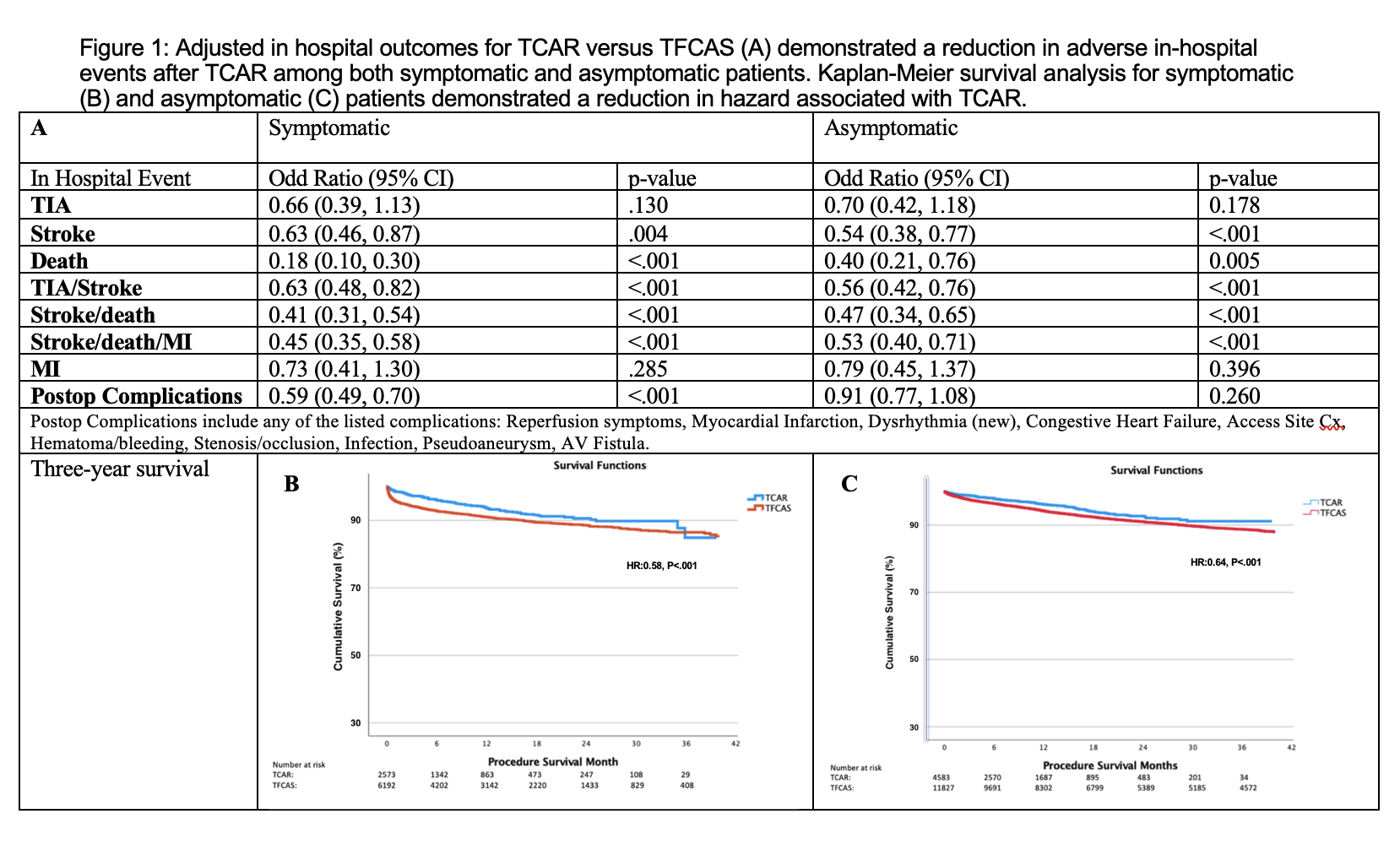
Back to 2022 Abstracts
