The Effect Of Transcarotid Artery Revascularization On Transfemoral Carotid Stenting And Carotid Endarterectomy Volume, Outcomes, And Practice
Charles DeCarlo, MD, Young Kim, MD, Samuel Jessula, MD, Jahan Mohebali, MD MPH, Anahita Dua, MBChB MBA MSc, Abhishek Mohapatra, MD.
Massachusetts General Hospital, Boston, MA, USA.
Background: Transcarotid Artery Revascularization (TCAR) has shown excellent perioperative outcomes, but it is unclear how TCAR is currently being utilized in practice. We sought to determine in which patients TCAR is being utilized and the effect of TCAR uptake on carotid endarterectomy (CEA) and transfemoral carotid stenting (tfCAS) volume.
Methods: Including centers that contributed to both VQI CEA and CAS datasets for 2013-2020, yearly TCAR/CEA/ tfCAS volume and perioperative stroke/death was assessed using the Cochran-Armitage test for trend. Comparisons of demographic and patient factors for TCAR compared to CEA and tfCAS were made using chi-squared/t-test.
Results: Among 46 centers (volume: 285-2965 cases), 46,507 interventions comprised of 3,196 (6.9%) TCAR, 7,273 (15.6%) tfCAS, and 36,038 (77.5%) CEA, ranging from 5,251-6,102 total yearly interventions (0.16). CEA and tfCAS both saw a significant decline in volume, comprising 81.0% and 18.2% of procedures in 2013 vs. 69.2% and 13.2% of procedures, respectively, in 2020 (CEA P<0.001; tfCAS p=0.002; Figure). Yearly stroke/death rate ranged from 1.9-2.5% with no significant trends (p=0.16). For the years 2017-2020, TCAR patients were older (TCAR: 72.5±9.2 years vs. tfCAS: 69.5±10.1 years and CEA: 70.7±9.4 years), more likely to be ASA class 4 (TCAR: 26.8% vs. tfCAS: 17.7% and CEA: 19.3%), and less likely to have private insurance than CEA and tfCAS patients (TCAR: 29.6% vs. tfCAS: 35.7% and CEA: 37.9% ; p<0.05 for all comparisons). TCAR patients were more likely to be symptomatic than CEA patients but less likely to be symptomatic than tfCAS patients (TCAR: 44.6% vs. tfCAS: 63.3% [p<0.001] and vs. CEA: 35.8% [p<0.001]).
Conclusion: TCAR has resulted in a decline in both CEA and tfCAS volume, with no observed change in overall carotid volume. TCAR is preferentially utilized in older patients with greater comorbidity burden, but not necessarily in symptomatic patients. The uptake of TCAR as a replacement for both CEA and tfCAS in a subset of patients has not led to any change in perioperative stroke/death rates. 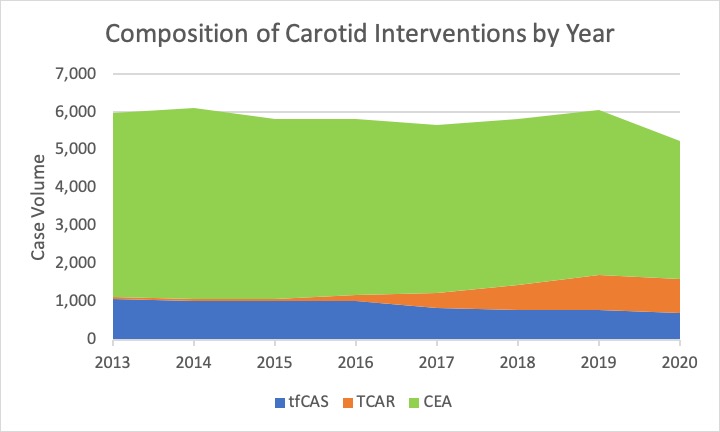
Back to 2022 Abstracts
