The Efficacy And Safety Of Single Versus Dual Antiplatelet Therapy In Carotid Artery Stenting
Christina L. Marcaccio, MD, MPH1, Priya B. Patel, MD, MPH1, Vinamr Rastogi, MD1, Lars Stangenberg, Md, PhD1, Patric Liang, MD1, Jeffrey Jim, MD2, Peter A. Schneider, MD3, Marc L. Schermerhorn, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Minneapolis Heart Institute at Abbott Northwestern Hospital, Minneapolis, MN, USA, 3University of California San Francisco, San Francisco, CA, USA.
OBJECTIVES: Current guidelines recommend dual antiplatelet therapy (DAPT) prior to carotid artery stenting (CAS), but the true clinical impact of single antiplatelet therapy (SAPT) versus DAPT is unknown. Therefore, we examined the efficacy and safety of preoperative SAPT versus DAPT in patients undergoing transfemoral CAS (tfCAS) or TCAR.
METHODS: We identified all patients undergoing tfCAS or TCAR in the VQI registry from January 2016-March 2021. We stratified patients by procedure and identified patients who received the following preoperative antiplatelet regimens: DAPT (ASA+P2Y12-inhibitor(P2Yi)), ASA only, P2Yi only, and ASA+P2Yi load (which was administered within 4 hours of CAS). We generated propensity scores for each treatment regimen and assessed outcomes using inverse probability-weighted log binomial regression with DAPT as reference group, also adjusting for intraoperative protamine use. The primary efficacy outcome was a composite endpoint of in-hospital stroke/death, and the primary safety outcome was access-related bleeding.
RESULTS: Among 17,731 tfCAS patients, 12,490(70%) received DAPT, 1783(10%) received ASA only, 811(4.6%) received P2Yi only, and 1508(8.5%) received ASA+P2Yi load. Unadjusted rates of stroke/death and access-related bleeding are presented in the Table. After adjustment, compared with DAPT, stroke/death was higher with ASA only (relative risk[RR] 1.5[95% confidence interval 1.1-2.0]) and with ASA+P2Yi load (RR 2.0[1.5-2.7]) but was similar with P2Yi only (RR 0.8[0.5-1.4])(Table). There were no differences in access-related bleeding across groups (Table).
Among 17,946 TCAR patients, 14,420(80%) received DAPT, 1045(5.8%) received ASA only, 866(4.8%) received P2Yi only, and 684(3.8%) received ASA+P2Yi load. Unadjusted rates of stroke/death and access-related bleeding are presented in the Table. After adjustment, compared with DAPT, stroke/death was higher with ASA only (RR 2.2[1.5-3.2]) and with ASA+P2Yi load (RR 1.8[1.0-3.2]) but was similar with P2Yi only (RR 1.1[0.6-2.2])(Table). There were no differences in access-related bleeding across groups (Table).
CONCLUSIONS: Compared with preoperative DAPT, ASA monotherapy and ASA with preoperative P2Yi loading was associated with higher risk of stroke/death but similar bleeding risk after CAS. These findings support current guidelines recommending DAPT prior to CAS but also suggest that P2Yi monotherapy may confer similar thromboembolic benefits, while P2Yi loading within 4 hours of CAS may not provide additional thromboembolic protection. 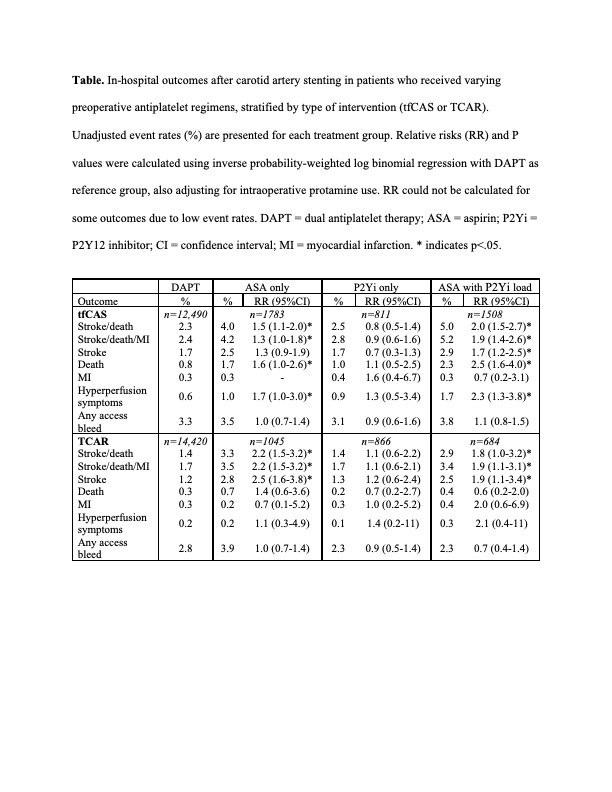
Back to 2022 Abstracts
