Using Ultrasound Elastography To Detect Changes Of Aortic Strain In Patients Following Abdominal Endovascular Aneurysm Repair
Zachary R. Zottola, B.S., Dakota W. Gonring, B.A., Maxwell L. Wang, B.S., Michael S. Richards, PhD., Michael C. Stoner, M.D., Doran S. Mix, M.D..
University of Rochester Medical Center, Rochester, NY, USA.
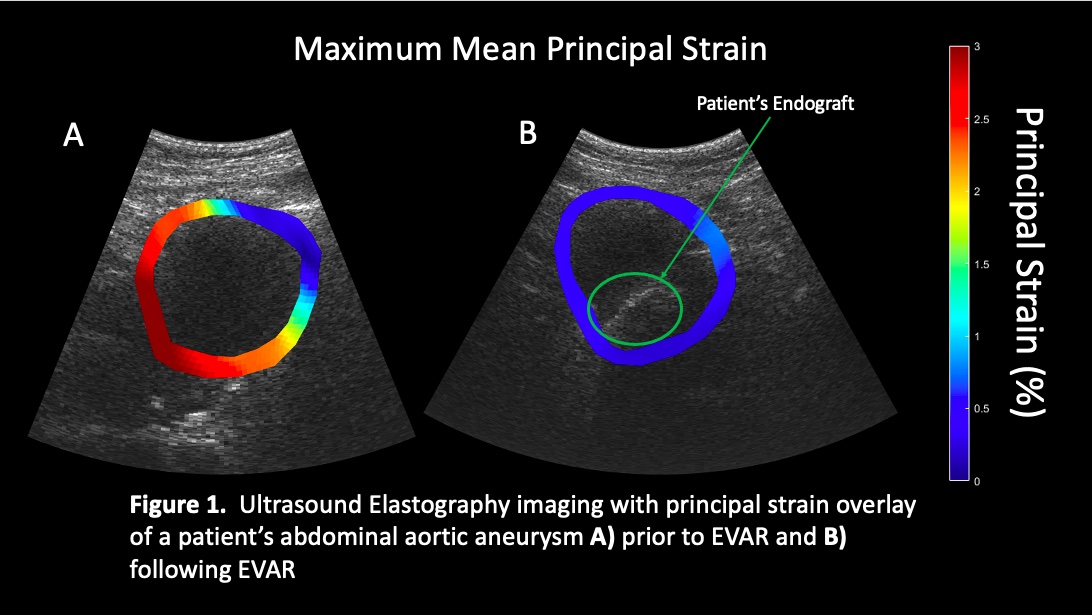
OBJECTIVE: Standardized practice for predicting success following endovascular aneurysm repair (EVAR) of abdominal aortic aneurysms (AAA) relies on measurements of diameter and growth rate, assessed mainly by postoperative computed tomography angiography (CTA). These metrics alone are insufficient to reliably predict the stability of AAA. Biomechanical properties such as strain may provide useful information in assessing patient AAA following EVAR. Our objective was to assess the feasibility of a using a novel ultrasound elastography technique (USE) to detect changes of aortic wall strain in patients undergoing EVAR. METHODS: Ten patients were imaged both preoperatively and postoperatively using USE. Mean principal strain (ερ+ ) for each scan was assessed using our novel technique, which employs a finite element mesh to track multiple frame-to-frame displacement fields of a 2D, axial image of the aorta, over an entire cardiac cycle. This was then divided by the pulse pressure taken at the time of the scan, to produce a pressure-normalized strain measurement (ερ+ /PP). Two-tailed paired T-test was used to compare preoperative and postoperative ερ+ /PP. Aneurysmal sac regression and endoleak data were collected via chart review on a subset of seven patients for which 30-day follow-up data was available. RESULTS: Analysis of USE imaging demonstrated a significant reduction in average ερ+ /PP (0.227%/kPa ± 0.137%/kPa versus 0.076%/kPa ± 0.036%/kPa; p= 0.008, Fig. 1) from preoperatively to postoperatively. Follow up data showed two patients with type II endoleaks, one of which required a subsequent revision. The patient requiring revision was found to have the smallest reduction in ερ+ /PP (0.016%/kPa) with a sac regression of 1.8 mm. Interestingly, the second patient presenting with endoleak was found to have the largest reduction in ερ+ /PP (0.248%/kPa) and largest sac regression (3.8 mm). All remaining patients showed both notable ερ+ /PP reduction and favorable sac regression (mean = 1.42 mm±1.39 mm). CONCLUSION: Our analysis demonstrates the USE technique employed is a feasible method for detecting significant reductions in ερ+ /PP following EVAR in clinical patients. Further investigation is needed to assess the ability of USE to detect significant endoleaks. However, this preliminary data shows promising correlates between ερ+ /PP and favorable AAA remodeling, suggesting this methodology could potentially replace the need for postoperative CTA scan.
Back to 2022 Abstracts
