Outcomes Of Low And Standard-profile Fenestrated And Branched Stent-grafts For Treatment Of Pararrenal And Thoracoabdominal Aortic Aneurysms
Marina Dias-Neto1, Emanuel R. Tenorio1, Guilherme BB Lima1, Aidin Baghbani-Oskouei1, Naveed Saquib1, Bernardo C. Mendes2, Aleem K. Mirza1, Gustavo S. Oderich1.
1The University of Texas Health Science Center at Houston, Houston TX, TX, USA, 2Division of Vascular and Endovascular Surgery, Mayo Clinic, Rochester, MN, USA.
OBJECTIVES: To compare outcomes of fenestrated-branched endovascular repair (FB-EVAR) using low-profile (LP) and standard-profile (SP) stent-grafts for complex aortic aneurysms.
METHODS: We retrospectively reviewed 466 consecutive patients (70% male; mean 74±8 years-old) enrolled in a prospective nonrandomized study to investigate FB-EVAR for treatment of PRA and TAAAs (2013-2021). Endpoints were compared in patients treated with LP (18-20F) and SP (22F) devices, including procedural metrics, access-related complications, major adverse events (MAE), patient survival, freedom from secondary intervention and aneurysm sac enlargement.
RESULTS: There were 278 complex abdominal and 188 Extent I-III TAAAs treated by FB-EVAR, with mean of 3.9±0.5 vessels/patient. LP devices were used in 239 patients (51%) and SP in 227 patients (49%). LP devices were used more frequently for chronic dissections (12% vs 7%; P=.041) and with preloaded systems (77% vs 65%; P=.005) and bilateral percutaneous access (83% vs 74%, P.020), and less frequently with upper extremity access (67% vs 88%, P<.001). There was no difference in need for iliac conduits for LP and SP devices (8% vs 10%, P=.322). Patients treated by LP devices had similar technical success (96% vs 97%; P=.527), but lower total operating time (225±81 vs 164±60 min; P=.018) and radiation exposure (1.4±1.1 vs 1.3±1.9 Gy; P<.001). There was no difference in iliofemoral access complications for patients with LP and SP devices (1.3% vs 3.5%, P=.107). At 30-days, mortality and MAE occurred in five (1%) and 91 patients (28%), with no differences between groups. Mean follow-up was 29 months (95%CI 27-31 months). At 4-years, patients treated by LP devices had similar freedom from all-cause mortality (70%±6% vs 67%±4%, P = .485), freedom from aortic-related mortality (97%±1% vs 98%±1%, P = .475), freedom from any secondary intervention (89±2% v 92±2%, P =.173) and freedom from aneurysm sac enlargement (90±6% vs 95±2%, P=.282). Cumulative risk of sac regression or stabilization was higher in patients treated with LP devices (P < 0.001) (Figure 1). CONCLUSIONS: LP devices were used more often with preloaded systems and had lower total operation time and radiation exposure, with no difference in mortality, MAEs, patient survival, freedom from secondary interventions and sac enlargement. 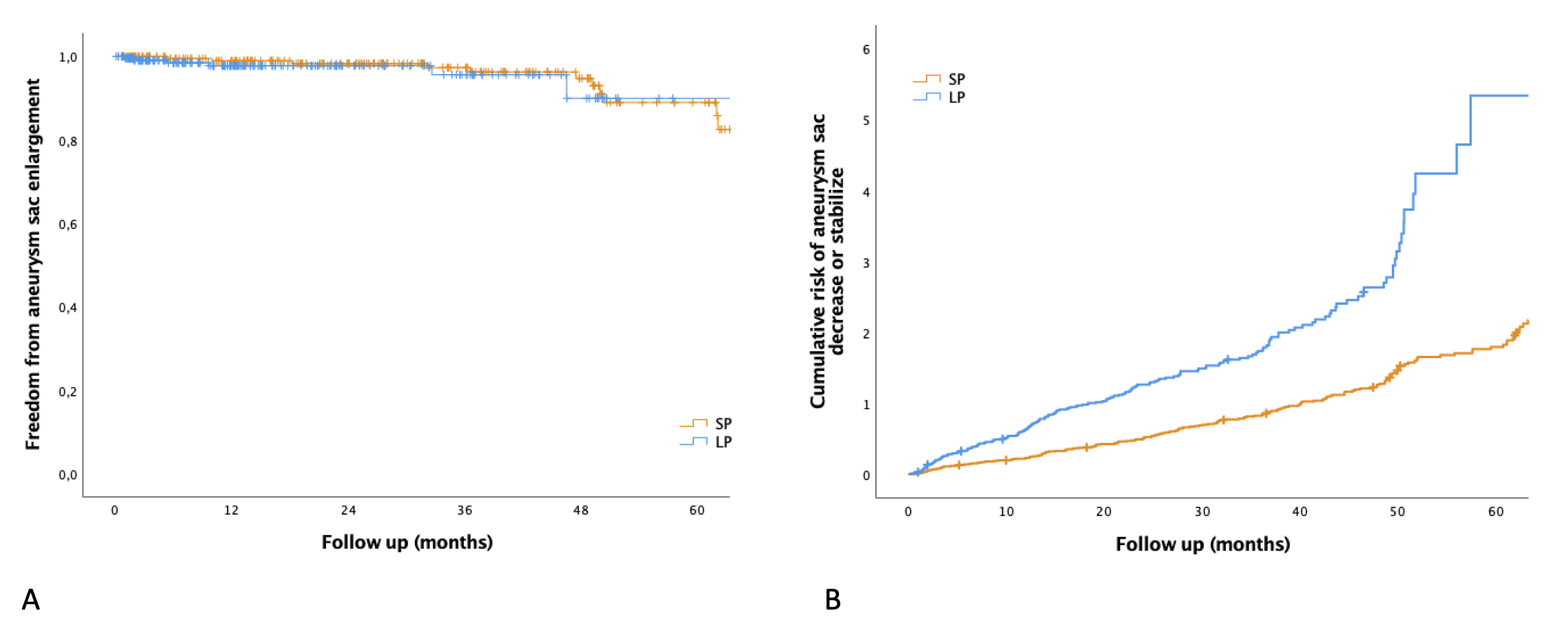
Back to 2022 Abstracts
