The Impact Of Neighborhood Social Disadvantage On Abdominal Aortic Aneurysm Presentation And Management
Lucas Mota, MD1, Christina L. Marcaccio, MD1, Priya B. Patel, MD1, Aderike Anjorin, MPH1, Peter A. Soden, MD2, Carla C. Moreira, MD2, Kakra Hughes, MD3, Marc L. Schermerhorn, MD1.
1Division of Vascular and Endovascular Surgery, Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Division of Vascular Surgery, Alpert Medical School of Brown University, Providence, RI, USA, 3Division of Vascular Surgery, Howard University College of Medicine, Washington, DC, USA.
Objective: Recent studies have highlighted socioeconomic disparities in the presentation and management of abdominal aortic aneurysm (AAA) disease. However, these studies focus on individual measures of social disadvantage such as income and insurance status. Area Deprivation Index (ADI), a validated measure of neighborhood adversity, provides a more comprehensive assessment of social disadvantage. Therefore, we examined the impact of ADI on AAA severity and its management.
Methods: We identified all patients who underwent EVAR or open repair of an AAA in the VQI registry between 2003-2019. An ADI score of 1-100 was assigned to each patient based on their residential zip code, with higher ADI scores corresponding with increasing adversity. Patients were categorized by ADI quintiles. Outcomes of interest included rates of rAAA repair (vs intact repair) and rates of EVAR (vs open repair). Logistic regression was used to evaluate for an independent association between ADI quintile and these outcomes.
Results: Among 55,931 patients who underwent AAA repair 6,649 (11.9%) were in the lowest ADI quintile, 11,692 (20.9%) in the second, 15,958 (28.5%) in the third, 15,035 (26.9%) in the fourth and 6,597 (11.8%) in the highest ADI quintile. Patients in the two highest ADI quintiles had a higher proportion of rAAA repair compared with those in the lowest ADI quintile (8.9% and 9.1% vs 6.2%, p<0.001). They were also less likely to undergo EVAR when compared with the lowest ADI quintile (81.3% and 80.8% vs. 87.5%, p<0.001). There was an overall trend toward increasing rAAA and decreasing EVAR rates with increasing ADI quintiles (Figure). In adjusted analyses, when compared with patients in the lowest ADI quintile, patients in the highest ADI quintile had higher odds of rAAA repair (OR 1.47, 95%CI 1.24-1.75, p=0.005) and a lower odds of undergoing EVAR (OR 0.67, 95%CI 0.59-0.77, p<0.001).
Conclusions: Among patients who underwent AAA repair in the VQI, those with higher neighborhood adversity had significantly higher rates of rAAA repair and lower rates of EVAR. Further work is needed to better understand neighborhood factors that are contributing to these disparities in order to identify community-level targets for improvement 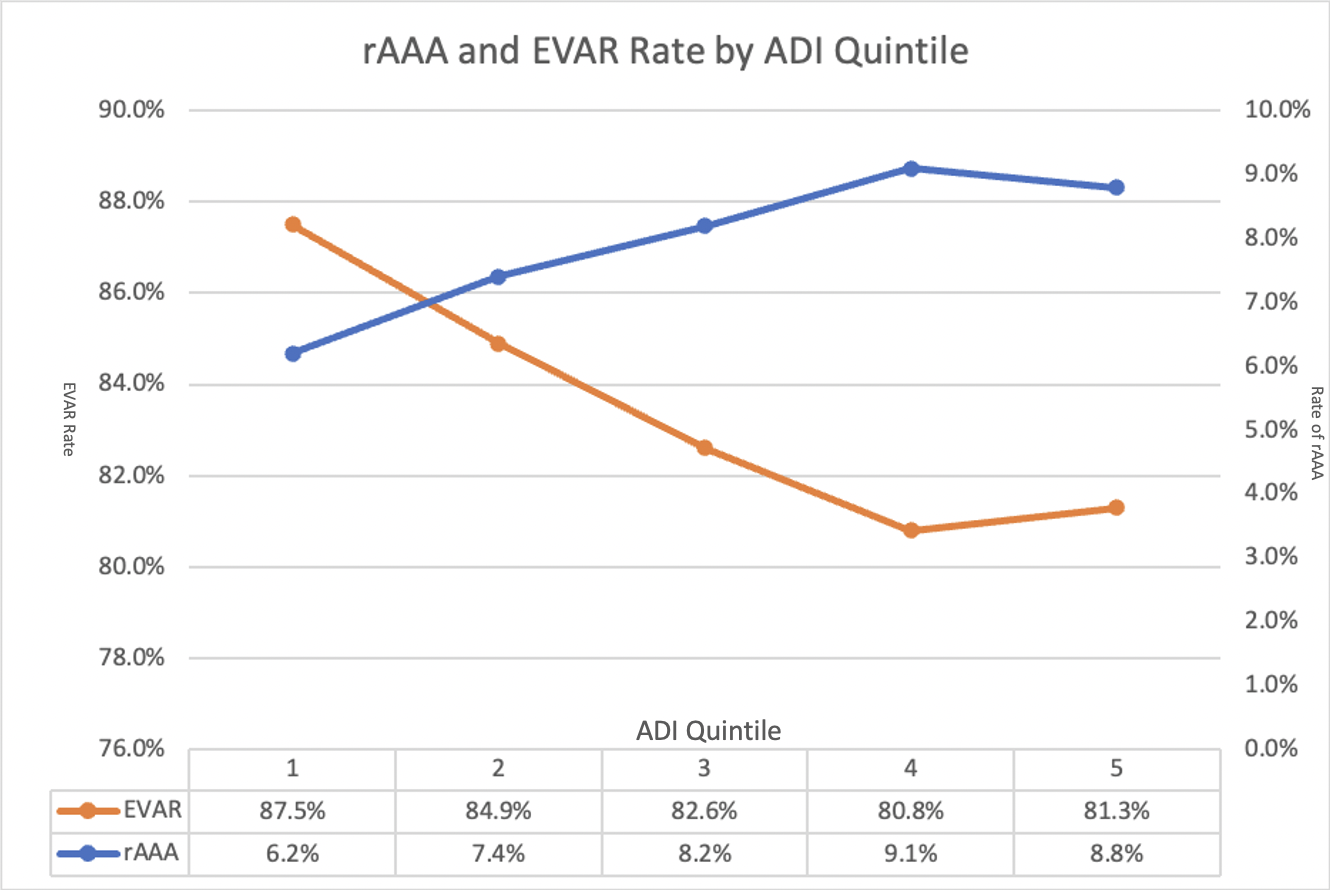
Back to 2022 Abstracts
