The Impact Of Optimal Medical Therapy On Long-Term Outcomes After Infrainguinal Bypass
Sophie X. Wang, MD1, Christina L. Marcaccio, MD, MPH1, Priya B. Patel, MD, MPH1, Peter A. Soden, MD2, Douglas W. Jones, MD3, Marc L. Schermerhorn, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Brown University, Providence, RI, USA, 3UMass Memorial Health, University of Massachusetts, Worcester, MA, USA.
Objectives: Despite current guidelines recommending antiplatelet and statin therapy after lower extremity revascularization, optimal medical therapy (OMT) is underutilized in vascular patients. Our aim was to study the effect of OMT at discharge on major adverse limb events (MALE) and mortality following infrainguinal bypass.
Methods: We identified patients who underwent infrainguinal bypass for symptomatic PAD in the VQI-Medicare linked database from 2003-2017 with follow-up through 2018. OMT was defined as discharge on both an antiplatelet agent and a statin. Outcomes of interest were 5-year MALE (reintervention or major amputation) and mortality. We compared outcomes in patients discharged with or without OMT using Kaplan-Meier and Cox regression analyses. We also assessed outcomes stratified by disease severity (claudication or CLTI) and explored the effect of antiplatelet therapy or statin therapy alone compared with OMT.
Results: Among 12556 patients, 9579(76%) received OMT at discharge and 2977(24%) did not. At 5 years, there were no differences in rates of MALE (OMT:72% vs non-OMT:72%; unadjusted hazard ratio[uHR] 1.0[0.95-1.1]) or reintervention (68% vs 67%; uHR 0.98[0.92-1.0]). However, 5-year major amputation and mortality rates were significantly higher in the non-OMT group (amputation: 20% vs 23%, uHR 1.2[1.0-1.23]; mortality: 48% vs 55%, uHR 1.3[1.2-1.3]). After adjustment, non-OMT was independently associated with higher risk of amputation (adjusted HR[aHR] 1.2[1.0-1.3]) and mortality (aHR 1.2 [1.1-1.3]). Non-OMT trended towards higher risk of MALE (aHR 1.1[0.99-1.2]) and reintervention (aHR 1.1[0.99-1.2]) (Table). In subgroup analysis, non-OMT at discharge was associated with higher risk of all endpoints in CLTI patients (MALE: aHR 1.1[1.1-1.2]; amputation: aHR 1.2[1.1-1.4]; reintervention: aHR 1.1[1.0-1.2]; mortality: aHR 1.2[1.1-1.3]), but was only associated with higher mortality in claudicants (aHR 1.2[1.0-1.5])(Table). Patients receiving an antiplatelet or a statin alone had higher mortality rates than those receiving OMT (statin only: aHR 1.2[1.0-1.4]; antiplatelet only: aHR 1.2[1.0-1.3]; neither: aHR 1.0[0.8-1.1]).
Conclusions: Patients not prescribed OMT after lower extremity bypass have inferior limb outcomes and survival, particularly those who present with CLTI. OMT provides a survival benefit over antiplatelets or statins alone. Further studies are warranted to understand factors contributing to OMT underuse in this population despite evidence of clinical benefit. 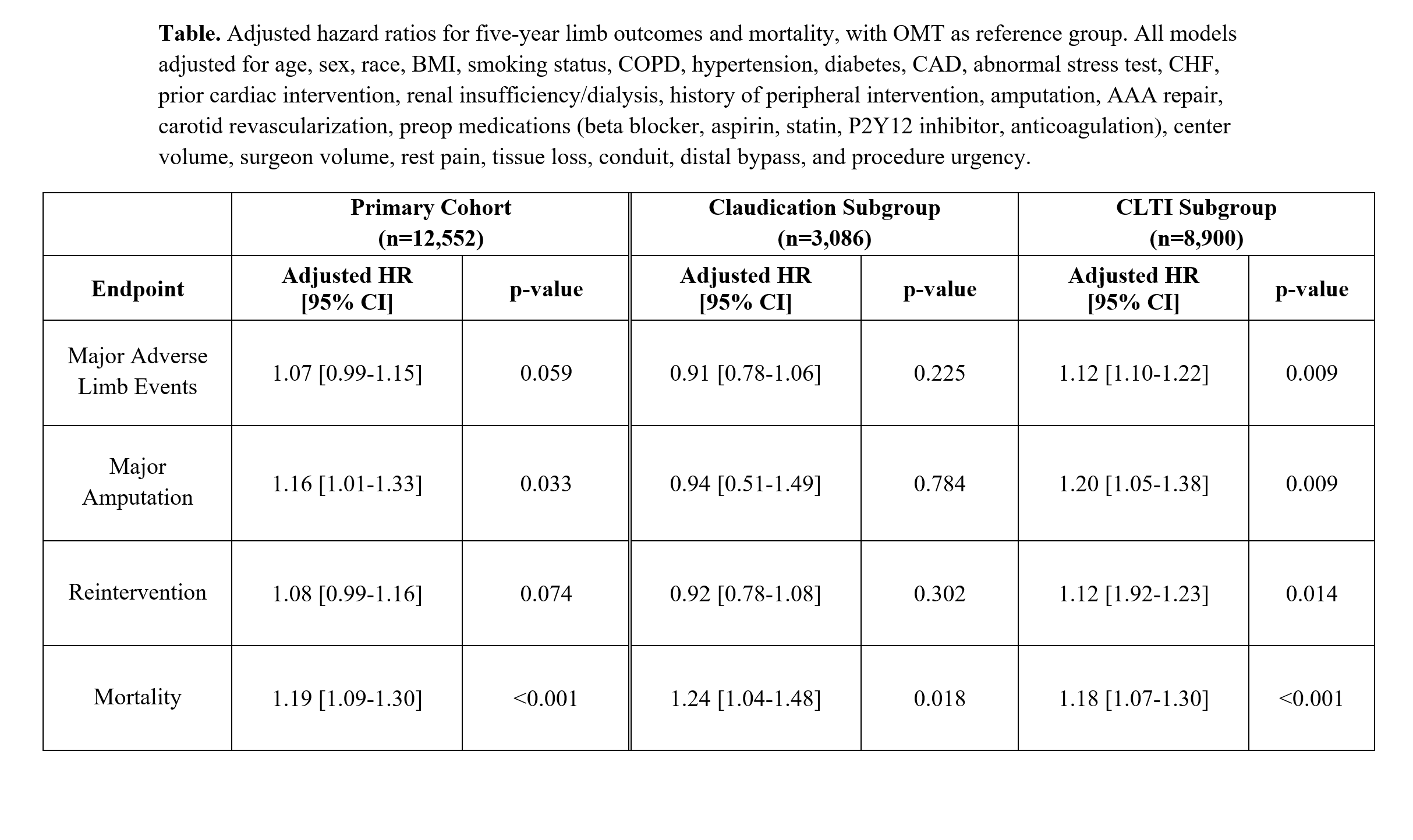
Back to 2022 Abstracts
