Analysis Of Bleeding Complications In Patients On Anticoagulation Undergoing Endovascular Intervention: A Tertiary Center Experience
Lucille Yao, MD, Willis Wagner, MD, Rajeev Rao, MD, Ryan A. Haqq, MD, Rameen Moridzadeh, MD, Allan Tulloch, MD.
Cedars-Sinai Medical Center, Los Angeles, CA, USA.
OBJECTIVES: Current convention is to hold anticoagulation prior to endovascular procedures to prevent hemorrhage. However, to date, no study has characterized the risk of hemorrhage for patients on anticoagulation undergoing elective endovascular interventions. We hypothesized that patients on preoperative anticoagulation and antiplatelet agents may continue their regimen without increased risk of major hemorrhage.
METHODS: We conducted a retrospective review of all adult patients undergoing elective lower extremity angiography or EVAR from January 2017 to March 2019. Type of anticoagulation at the time of procedure including none, antiplatelet therapy, or full anticoagulation were documented and compared. Type of closure was also noted. The primary endpoint was operative re-intervention for bleeding within 30 days. Secondary endpoints included 30-day all cause re-operation, emergency department visits, and postoperative length of stay. Fisherís Exact Test, Chi-squared Test, and Studentís T-test were used to compare outcomes.
RESULTS: During the study period, 203 patients underwent endovascular arterial intervention. 154 patients were on preoperative antiplatelet agents and/or therapeutic anticoagulation (Group AC) and 49 patients were not on either (Group NAC). 26 patients underwent EVAR, so 229 total limbs were accessed. Patients in Group AC had more comorbidities, but the groups were similar in operative characteristics. Only one patient required operative re-intervention (Group AC n=1, 0.58% vs. Group NAC n=0; p=1). No significant differences between groups were found in terms of our secondary endpoints. Within Group AC, 47 patients (50 limbs accessed) were on therapeutic anticoagulation (Group TAC). No patients required re-operation for bleeding within Group TAC, and there were no significant differences between groups in terms of secondary endpoints.
CONCLUSIONS:
In summary, we found that uninterrupted continuation of anticoagulation and/or antiplatelet agents through the perioperative period did not result in an increased risk of operative intervention for bleeding, length of stay, or adverse surgical outcomes compared to patients who were not on anticoagulation. Further study with larger cohorts will be necessary to better define safety. 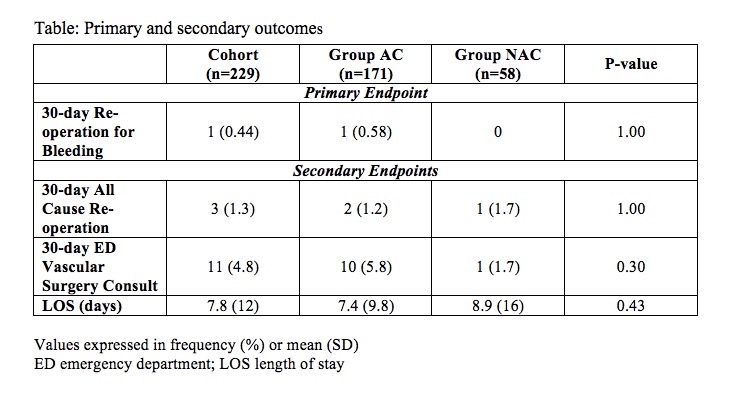
Back to 2022 ePosters
