Transcarotid Artery Revascularization For A High-Risk VA Population
Kenneth R. Nakazawa, MD, Jessica Ding, BA, Johnathan Allen, MCMSc, Harry Schanzer, MD, Rajiv K. Chander, MD.
James J. Peters Veterans Affairs Medical Center, Bronx, NY, USA.
OBJECTIVES: To report the safety and efficacy of performing transcarotid artery revascularization (TCAR) procedures for a high-risk veteran population at a Veterans Affairs (VA) Medical Center (VAMC).
METHODS: We retrospectively analyzed patients who underwent TCAR at the James J. Peters VAMC (Bronx, NY) from 2019-2021. Patient demographics, preoperative history, lesion characteristics, and procedural considerations were evaluated. Postoperative outcomes and follow-up data were reviewed.
RESULTS: From 2019-2021, 46 consecutive patients underwent 52 total TCAR procedures. Preoperatively, all patients took aspirin, clopidogrel (dual antiplatelet therapy) and high-intensity statin for >5 days. The cohort was predominantly male (98.1%) with median age 73.5 years (interquartile range, IQR 71-82.5) and high anatomic (59.6%) or physiological (76.9%) risk features for undergoing carotid endarterectomy (CEA). Of the lesions, 30.8% were considered symptomatic, and 11.1% had calcium thickness >3mm. Circumferential calcium was observed in 4.4% of cases, none wider than 3mm. General anesthesia was used for all procedures. Lesions were pre-dilated with median balloon diameter of 5mm (IQR 5-6) and the ENROUTE stent was used with median stent diameter and length of 10mm (IQR 9-10) and 40mm (IQR 40-40), respectively. Protamine was always administered for heparin reversal. There was 100% acute device and technical success. Postoperative anemia and hematomas were rare (1.9%) with no observation of permanent cranial nerve injury. With a median follow-up period of 347 days (IQR 123-510), the 30-day stroke, myocardial infarction (MI), and death rates were 0%, 1.9%, and 3.9%, respectively (composite outcome: 3.9%). One death was attributed to fatal MI on postoperative day (POD) 1 and another to COVID-19 pneumonia on POD27 (discharged on POD2). Four 30-day readmissions (7.7%) were individually due to atrial fibrillation, shortness of breath, COVID-19 and hyperglycemia. Stroke rate at 1-year remained 0%, and 1-year follow-up imaging showed 100% primary patency.
CONCLUSIONS: We offered TCAR to high-risk VA patients as an alternative to CEA or trans-femoral carotid stenting (TF-CAS). Perioperative and short-term outcomes appear comparable to reports in TCAR clinical trials and historical controls of CEA/TF-CAS. While long-term analysis is needed, data suggests TCAR is safe and effective for management of carotid artery occlusive disease among the VA population. 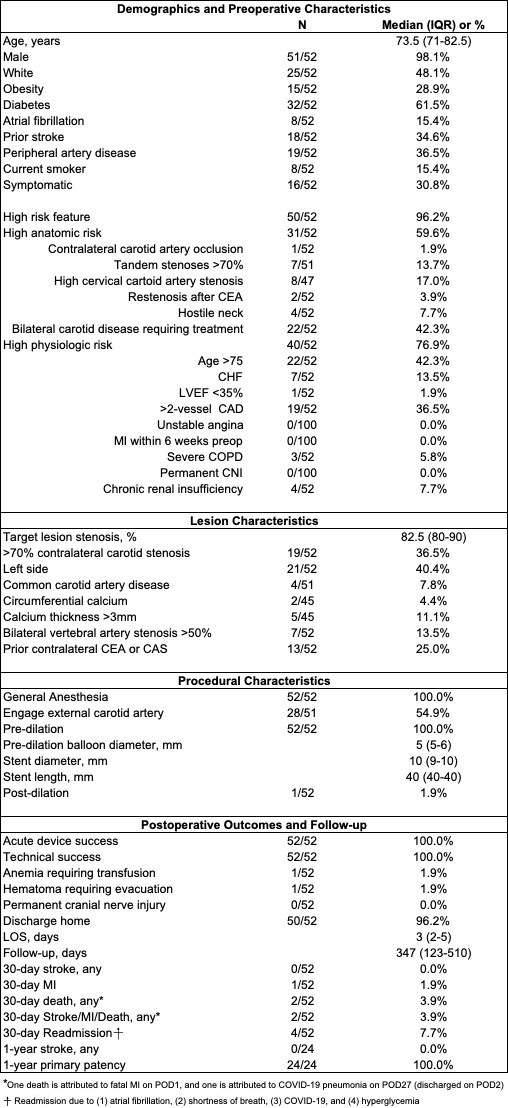
Back to 2022 ePosters
