Ethnicity And TEVAR Outcomes
Peter V. Cooke, BA1, Justin M. George, MD2, Halbert Bai, MPH1, Ajit Rao, MD2, Michael L. Marin, MD2, Peter L. Faries, MD2, Rami O. Tadros, MD2.
1Icahn School of Medicine at Mount Sinai, New York, NY, USA, 2Division of Vascular Surgery, Mount Sinai Hospital, New York, NY, USA.
Objective: Studies reporting outcomes based on patient ethnicity for aortic interventions are sparse. This study’s objective was to determine the rate of complication, reintervention, and short-term mortality based on self-reported patient ethnicity.
Methods: A single-institution prospectively maintained database of patients undergoing TEVAR from August 2001 to January 2020 was analyzed. Patients were separated into five cohorts based on self-reported ethnicity: African American, Asian, Caucasian, Hispanic, and Other. SVS guideline standards were used to report intraoperative, in-hospital, and post-discharge complications. Reinterventions associated with the index TEVAR procedure were assessed. Asian patients were excluded from logistic regression analysis for 30-day mortality, as no patients from this cohort died within the first 30-days
Results: Among 310 patients fitting the study criteria, we identified 63 African American, 18 Asian, 156 Caucasian patients, 36 Hispanic, and 37 Other patients. Mean age at surgery differed between cohorts- African American: 66.3, Asian: 66.3, Caucasian: 71.5, Hispanic: 68.4, and Other: 66.8 (p=0.001). Diabetes prevalence varied across cohorts, with Hispanics as the highest (30.6%) (p<0.001). Caucasians and African Americans had the highest rates of known AAA history (31.4% and 28.6%, respectively, p=0.020). Other demographics and comorbidities were similar across cohorts. The distribution of TEVAR indications was significantly different across the five cohorts, with African American patients presenting with the highest proportion of type b aortic dissections (32.4%) and Caucasian patients with the highest proportion of thoracic aortic aneurysm (65.3%) (p=0.049). Intraoperative, in-hospital, and post-discharge complication rates, including rates of spinal cord ischemia, did not significantly differ between ethnicities. Time to reintervention and odds of reintervention were not significantly different across cohorts. There was no significant difference in reintervention-free survival (p=0.90). Odds of thirty-day mortality were not significantly different on univariate or multivariable analysis. (Table).
Conclusion: There appear to be differences in primary indication for TEVAR based on self-reported patient ethnicity. Complications and short-term mortality did not differ across groups. Mean follow-up was lower for Asian and Hispanic patients, which warrants further investigation. 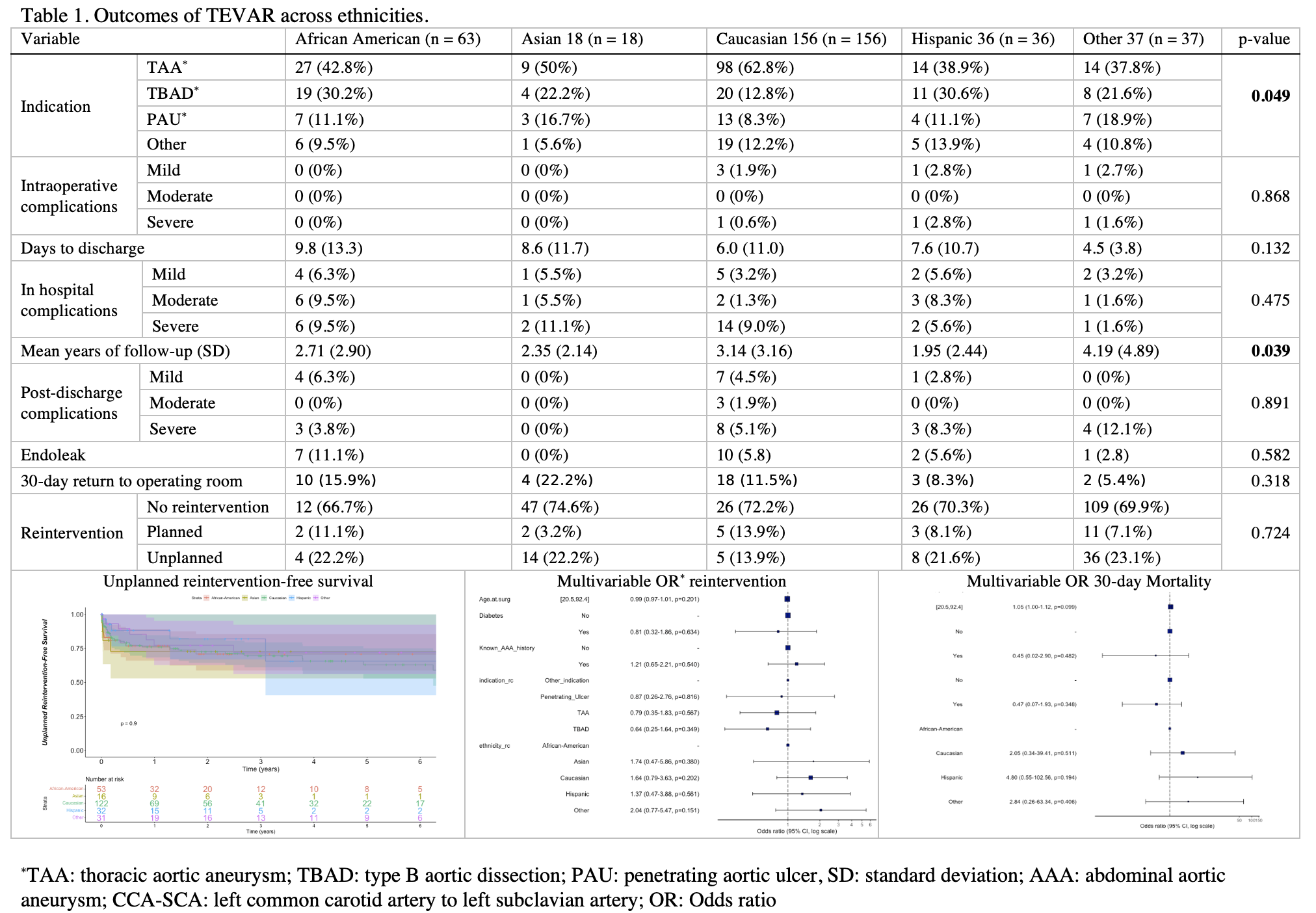
Back to 2022 ePosters
