30-day Outcomes After Aortobifemoral And Axillobifemoral Bypasses
Kenneth R. Nakazawa, MD, Rami O. Tadros, MD, Windsor Ting, MD, Peter L. Faries, MD, Ageliki G. Vouyouka, MD.
Mount Sinai Hospital, New York, NY, USA.
Objectives: To compare contemporary, short-term outcomes between aortobifemoral (AortoBiFem) and axillobifemoral (AxBiFem) bypasses for aortoiliac occlusive disease (AIOD)
Methods: Using 2012-2016 NSQIP vascular-targeted databases, we compared demographics, procedural characteristics, and 30-day outcomes between patients who had AortoBiFem vs AxBiFem. Yearly time-trends were investigated using linear regression. Independent factors associated with 30-day outcomes were determined by logistic regression.
Results: 969 AortoBiFem and 249 AxBiFem elective bypasses were identified (total 1218). There was a slowly increasing trend in AxBiFem (P=0.035), but no difference in ratio of AortoBifem to AxBifem over the 5 years (P>0.05). On univariate analysis, the AortoBifem cohort had younger patients, more admitted from home, independent-functioning, current smokers, and claudicants (P<0.05). The AxBifem cohort had more females, medical comorbidities, (CHF, COPD, dialysis-dependence, ASA-score ≥4), high-risk physiological factors, high-risk anatomical factors (prior abdominal surgeries, bypasses, and percutaneous interventions involving same segments) and chronic limb-threatening ischemia. Median operating time and LOS for AortoBifem vs AxBiFem were 260 vs 211 minutes and 7 vs 5 days, respectively (P<0.05). Univariate analysis of unmatched AortoBiFem and AxBiFem cohorts demonstrated 30-day mortality of 2.5% vs 4.0%, major adverse limb events (MALE) of 5.4% vs 6.8% and major adverse cardiac events (MACE) of 6.3% vs 6.8%, respectively (P>0.05). After adjusting for covariates, AortoBiFem was independently associated with lower untreated loss of patency (OR 0.20) and readmission rates (OR 0.52), but more pulmonary complications (OR 2.88) and bleeding requiring transfusion (OR 2.75) than AxBiFem (P<0.05). After multivariate logistic regression, there were no differences in 30-day mortality, re-intervention, amputation, MI, stroke, wound, renal, urinary, septic complications, or DVT rates. Sub-group analysis of females, non-white, or diabetic patients didnít identify different significant risk factors for complications for either procedure. Prior open or endovascular interventions didnít independently increase mortality (P>0.05).
Conclusions: Over the 5 years, there were approximately 4 times more AortoBiFem than AxBiFem. The annual number of AortoBiFem procedures remained stable with real-world 30-day mortality lower than historical controls. Short-term patency and readmission rates were also better than AxBiFem. These data suggest AortoBiFem reconstruction in the modern era remains an effective and safe procedure for the management of advanced AIOD. 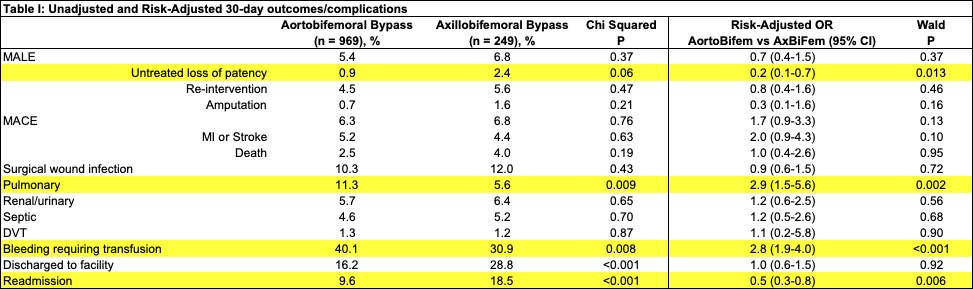
Back to 2022 ePosters
