Evaluating Hypoalbuminemia As A Predictive Tool For Post-operative Outcomes In Patients Undergoing Open Lower Extremity Revascularization Procedures
Lily S. F. Adler, BA1, Emann M. Rabie, PhD2, Anoop Alla, MS2, Samantha M. Shave, BS2, Saum A. Rahimi, MD1, William E. Beckerman, MD1.
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, USA, 2Rutgers Robert Wood Johnson Medical School, Piscataway, NJ, USA.
OBJECTIVES: We sought to investigate whether preoperative hypoalbuminema is associated with mortality and major adverse limb events (MALE) in patients undergoing open lower extremity revascularization procedures, whereas prior studies have shown conflicting results. In this study, we sought to find the maximal cut-off point for using albumin as a prognostic indicator of MALE and/or death in patients undergoing any open lower extremity vascular surgery.
METHODS: We conducted a retrospective analysis of a prospectively maintained database of patients who underwent open lower extremity revascularization procedures from January 2011 to January 2013 (N=179). Preoperative albumin was collected as close to the date of surgery as possible and no more than six months prior to surgical date. Primary outcomes were MALE or death. The maximally-ranked statistic method was used to determine the maximal albumin cut-off point. Kaplan-Meier analyses of death and MALE and albumin were used to compare the groups by albumin cut-off point. We conducted a multivariate analysis of the association between albumin and mortality using Cox proportional hazard models, including confounding variables such as age, smoking status, and hypertension. P-values <0.05 were considered statistically significant.
RESULTS: Fifty-eight patients undergoing surgery from January 2011 to January 2013 were analyzed. The median albumin level was 3.5 g/dL with IQR [2.8-3.9]. The analysis showed a negative correlation between hypoalbuminemia and mortality (P=0.005) and MALE (P=0.044) (Fig 1A and 1B) using the maximal cut-off point of 3.5 g/dL. Controlling for multiple comorbidities including, age, smoking, and gender, albumin was a significant independent predictor of mortality (P=0.022) and MALE (P=0.031). When controlling for diabetes, hypertension, and hyperlipidemia, albumin was also a significant independent predictor of mortality (P<0.001) and MALE (P=0.003) as was the albumin cut-off point for both death (P=0.004) and MALE (P= 0.028).
CONCLUSIONS: This study suggests that low albumin is an independent and useful predictor of mortality and MALE in patients undergoing open lower extremity revascularization surgeries. However, these results are limited by the small sample size. Going forward, we plan to expand this study to include more recent patients to determine if our initial results continue to be significant. 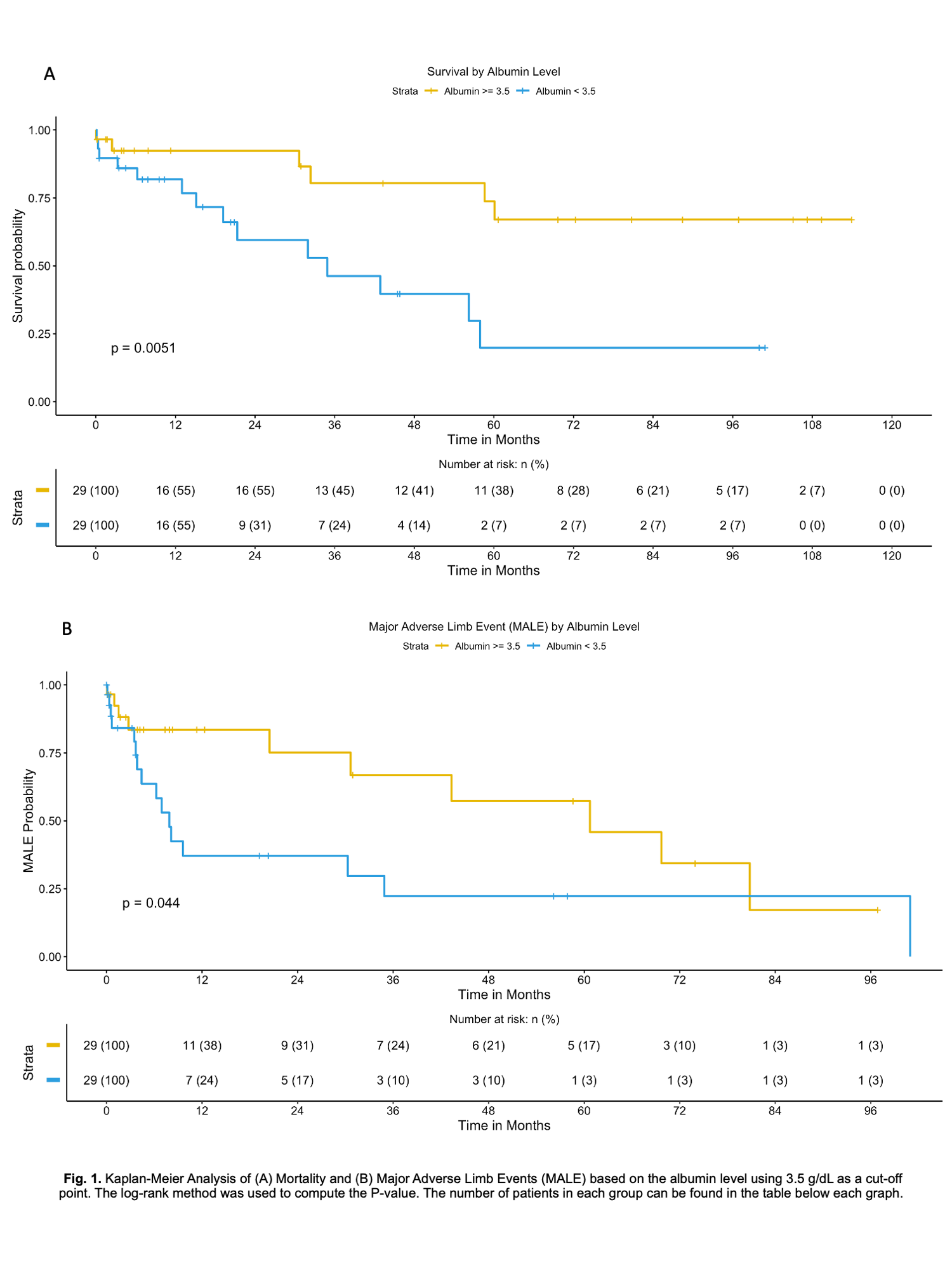
Back to 2022 ePosters
