Early Development Of Patient Specific 3d Modeling And Augmented Reality For Endovascular Treatment Of Aortic Aneurysms
Indrani Sen, Victoria Sears, Randall DeMartino, Todd Rasmussen, Jonathan Morris.
Mayo clinic, Rochester, MN, USA.
Introduction: Rapid technologic advances in CT Angiography (CTA), endovascular techniques, commercially available devices and hybrid operating rooms have led to significant decrease in morbidity and mortality related to abdominal aortic aneurysms (AAA). Similar technologic advancements in augmented reality (AR) has made intraoperative navigation a possibility. AR technologies require 3D computer- aided design (CAD) files to display patient-specific 3D data. Current 3D radiographic datasets are displayed using surface shaded displays limiting their use to 2D screens. Our aim was to build an ecosystem for improved aortic segmentation, 3D CAD file generation, and AR projection of patient-matched aortic segmentation via the cloud. Methods: After IRB approval, CTA of a patient with a AAA requiring treatment between 2019-2020 was identified. The CT data was anonymized, segmented, a Standard Tessellation Language (.STL) file created, and imported into Materialise 3-Matic for CAD optimization. The CAD file was exported in .OBJ file format and imported into MedReality AR system. A 3D printed model of the patientís skin surface and spine with a central viewing window to assure accuracy of AR coregistration was created using an Ultimaker S5 printer. The 3D segmented data set was then coregistered to the 3D printed model using surface fiducials as coregistration markers. Display of the 3D data sets in device neutral mobile platforms was then performed. Results: CTA data was segmented into 4 parts (skin, bone, cartilage, arteries) using Materialise Mimics. The .OBJ file format was uploaded to MedReality platform and distributed to 4 separate devices: HoloLens 2, iPhone 12, Samsung Galaxy phone and tablet, and iPad (8th Edition). All AR devices were able to accurate display the .OBJ in spatial and non-spatial AR conditions (Fig 1). The segmented 3D Data set was co-registered to the 3D printed patient model demonstrating preliminary acceptable accuracy rates. MedReality cloud-based distribution system was able to deploy the data on several mobile devices simultaneously. Conclusion: Integration of AR into vascular surgery has great promise. Use of cloud-based device neutral AR for patient education, treatment planning and endovascular treatment of aortic aneurysms may be paradigm to shortening a steep learning curves, reduced intraoperative radiation and improved outcomes. 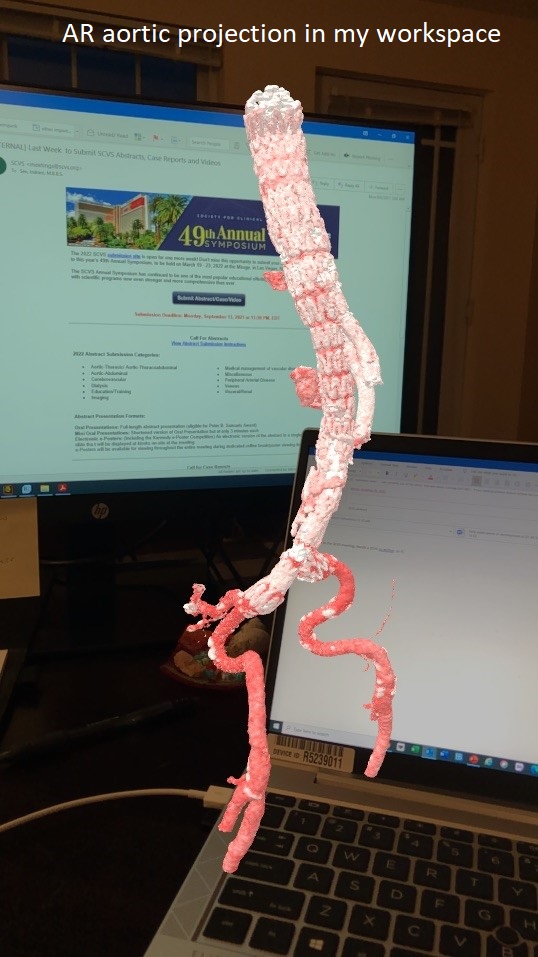
Back to 2022 ePosters
