Our Treatment Algorithm Using The Cook Bare Dissection Stents In Conjunction With Covered Stent Grafts Helps Promote Greater False Lumen Thrombosis And Aortic Remodeling Compared With Covered Stent Grafts Alone In All Types Of Type B Aortic Dissection
Michael Wilderman, MD, Anjali Ratnathicam, DO, David O'Connor, MD, Kristen Cook, MD, Yuriy Dudiy, MD, Elie Elmann, MD, Mark Anderson, MD, George Batsides, MD, Arthur NG, MD, Massimo Napolitano, MD, Gregory Simonian, MD.
Hackensack University Medical Center, Hackensack, NJ, USA.
OBJECTIVES: There has been increasing use of TEVAR for Acute Type B Aortic Dissections(TBAD).For Complicated TBAD,endovascular treatment is first line therapy.Recently,Cook Zenith Endovascular Dissection System was approved for commercial use.No consensus exists for uncomplicated TBAD,but evidence supports TEVAR to promote aortic remodeling and false lumen thrombosis.The use of the Uncovered Stent portion could lead to more true lumen expansion,false lumen thrombosis,and aortic remodeling without the risks of covered stents.
METHODS: Over 30 months,we placed 90 Cook dissection stents in conjunction with Covered Stent grafts in 43 patients for treatment of both complicated and uncomplicated TBAD. We reviewed our technical success(exclusion of the proximal tear),in-hospital,and 30-day mortality.We reviewed major adverse events (MAE)(MI, respiratory failure, bowel ischemia, stroke, renal failure, and paralysis) compared to historic controls with TEVAR without the bare dissection stent or open vascular repair.We followed patients for false lumen thrombosis,aortic size and re-intervention.
RESULTS: Following our treatment algorithm,33 male and 10 female underwent Endovascular repair of TBAD with both covered(multiple companies) and bare dissection stent(Cook Inc) placement. Indications were rupture(2 patients),malperfusion (9), aneurysmal degeneration(18),high risk radiographic features(12) and persistent pain(2). Technical success was 100%. The in-hospital and 30-day mortality was 5% (2 presenting with rupture).The incidence of MAE was 9% with CHF(1 patient),CVA(1),dialysis dependent renal failure(1), and infected femoral pseudoaneurysm(1). There was no paralysis.There were no subsequent deaths at 1 year. At a median follow up of 20 months, 100% showed either partial or total false lumen thrombosis. 2 patients(5%) showed increased aortic growth more than 5mm. One required a secondary procedure placing a covered stent at 22 months.
CONCLUSIONS: Using our treatment algorithm,30 day and 1 year ourcomes show favorable results using a combination of covered and bare dissection stents for the treatment of all TBAD. Moreover,the bare stents provide a longer treatment zone and promotes excellent false lumen thrombosis and aortic remodeling without the risks of covered stents. Our series demonstrates significantly more false lumen thrombosis using the bare stents in conjunction with covered stents, rather than covered stent grafts alone. While these results are promising, longer term data is required. 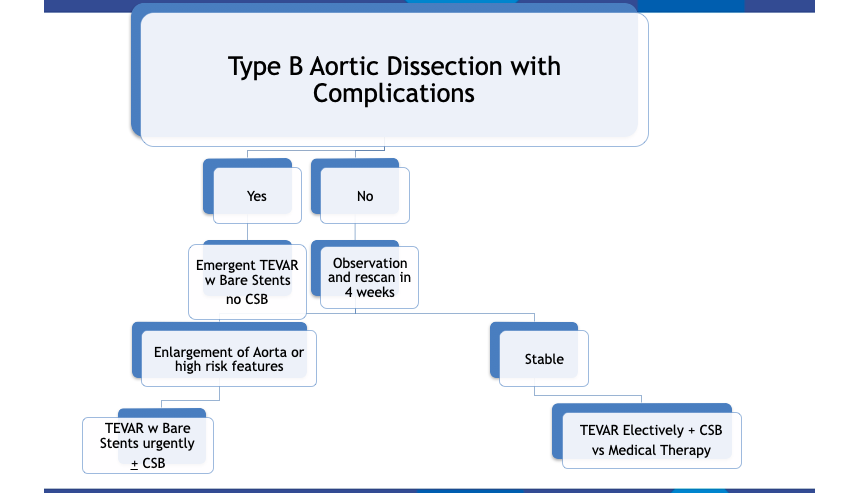
Back to 2022 ePosters
